The guidelines also recommend the use of immediate release opioids instead of extended release opioid medication and that doctors be cautious about prescribing doses higher than 50 morphine milligram equivalents (MME) per day. Doctors are strongly advised to avoid increasing doses over 90 MME per day.
For acute pain from injuries or medical procedures such as surgery, the CDC states that three days or less supply of opioids “often will be sufficient” and that 7 days supply “will rarely be needed.”
Doctors are also advised to consult prescription drug monitoring programs (PDMP) to determine if patients are abusing opioids or using dangerous combinations of medications. Urine drug testing is also recommended before starting opioid therapy and at least annually afterwards. The guidelines also discourage doctors from dropping patients if they fail to pass a drug test as that "could constitute patient abandonment and could have adverse consequences for patient safety."
The guidelines state that opioid pain medication and benzodiazepines should not be prescribed concurrently, and addiction treatment should be offered to patients who show signs of drug abuse.
“The new CDC guideline emphasizes both patient care and safety. We developed the guideline using a rigorous process that included a systematic review of the scientific evidence and input from hundreds of leading experts and practitioners, other federal agencies, more than 150 professional and advocacy organizations, a wide range of key patient and provider groups, a federal advisory committee, peer reviewers, and more than 4000 public comments.” Frieden wrote, without mentioning that the CDC initially sought very little input from the public or healthcare providers.
The CDC's own experts also admitted much of the evidence to support the guidelines was weak. The agency planned to implement the guidelines in January, but was forced to delay them after widespread criticism about its secrecy and lack of transparency during the drafting of the guidelines.
In response to critics, a new advisory committee was formed to review the guidelines, but after a handful of private meetings the committee endorsed the guidelines with few changes. A potential legal problem for the CDC is that none of its advisory committees' meetings were open to the public. The committees also reviewed the guidelines with outside consultants without publicly disclosing who they were.
Last year the Washington Legal Foundation (WLF) threatened to sue the agency for its “culture of secrecy” and “blatant violations” of the Federal Advisory Committee Act (FACA), which requires all such meetings to be open to the public.
"From the beginning we have been very disappointed in the manner CDC has conducted itself. We explained in detail last fall why we thought CDC had not acted in compliance with FACA. And while at first I was encouraged when CDC took steps to open up the process and perhaps try to compensate for some of its previous errors, I've seen nothing to suggest that it has really done so and in fact has just replaced one secret committee with another secret committee," said Richard Samp, WLF chief counsel. "I find it disappointing that a federal agency would not think it was incumbent to comply with federal law."
Samp told Pain News Network he was unsure if WLF would follow through on its threat to sue the agency and block the guidelines from being implemented.
"I can't say what if anything we plan to do from here or what anybody else plans to do," said Samp. "I just want to express our disappointment with the agency's procedural handling of this issue."
"We believe that this final version of the CDC guidelines leaves much to be desired," said Bob Twillman, PhD, Executive Director of the American Academy of Pain Management. "Looking across the two preliminary drafts and the final version, we see virtually no evidence that comments submitted by thousands of people with pain, patient advocacy organizations, and pain management societies resulted in any changes to the 12 recommendations in the guideline."
Twillman said he was concerned the "soft limits" on opioid dosages in the guidelines would be adopted as a rule by physicians, leaving some patients untreated or undertreated.
"Our concern is that, based on experience when states have implemented similar guidelines, some clinicians will interpret these 'soft limits' and thresholds as absolute ceiling doses, and that people with pain will suffer needlessly as a result," Twillman said.
"I don't see how they will contribute much to improved outcomes for people in pain," said Lynn Webster, MD, past president of the American Academy of Pain Medicine and Vice President of scientific affairs at PRA Health Sciences. " I wish the CDC would have advocated for the millions of Americans with chronic pain while also trying to curb the opioid crisis. We will never solve the opioid problem if we don't do a better job of treating pain.
"The CDC should have called upon Congress to insist payers be part of the solution and not continue to be the major barrier to improved outcomes for people in pain and with opioid addiction."
Many of the non-opioid treatments and therapies the CDC recommends -- such as cognitive behavioral therapy, massage and physical therapy -- are not covered by insurers.
"The CDC’s recommendations are very sound. They're pointing out that when opioids are used long term for chronic conditions they are more likely to harm patients than help. If you continue to take opioids daily for months and months, the opioids don’t work very well," said Andrew Kolodny, Executive Director and founder of Physicians for Responsible Opioid Prescribing (PROP), in an interview with KPCC Radio in Los Angeles.
PROP, which was heavily involved in the initial drafting of the guidelines, is funded by Phoenix House, a chain of addiction treatment centers that stand to benefit from the guidelines' recommendations.
"Opioids don't work well long-term. That's the CDC's message. That's what the evidence tells us. Its the industry and groups that get funding from industry that are promoting this inappropriate treatment," said Kolodny, who is chief medical officer of Phoenix House.
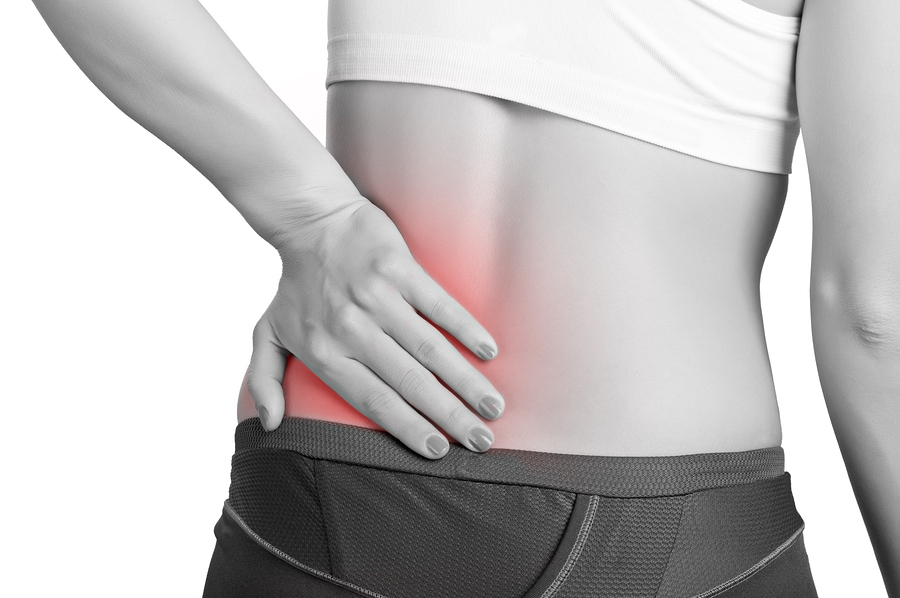
In a survey of over 2,000 pain patients by Pain News Network and the International Pain Foundation, many predicted the guidelines will lead to more opioid abuse and addiction, not less. Nearly 93% said they would be harmful to pain patients. Most also said that non-opioid treatments and therapies provide very little pain relief or none at all.