Prescription Opioids Play Minor Role in Massachusetts Overdoses
/By Pat Anson, PNN Editor
Two new studies in Massachusetts – one of the states hardest hit by the overdose crisis – highlight the role of multiple substances in most overdose deaths and how limiting the supply of prescription opioids has failed to reduce the number of drug deaths.
Researchers at Boston Medical Center's Grayken Center for Addiction analyzed toxicology reports on nearly 2,250 fatal overdoses involving opioids in Massachusetts between 2014 and 2015. Overdose data in Massachusetts is considered more reliable because it is one of the few states to extensively use toxicology testing.
Only 9 percent of the deaths in Massachusetts involved prescription opioids alone. Most of the overdoses (72%) involved illicit fentanyl or heroin, while one in five (19%) involved a combination of heroin, fentanyl or prescription opioids.
Other substances such as alcohol, marijuana, stimulants (cocaine and methamphetamine) and non-opioid medications (benzodiazepines and gabapentin) were also frequently involved.
“Using multiple substances, in addition to opioids, is the rule rather than the exception for opioid-related deaths,” researchers reported in the journal Drug and Alcohol Dependence.
“Our study draws attention to the heterogeneity of the problem at hand and that there is not a one-size-fits-all approach to addressing the overdose epidemic, which is increasingly driven by polysubstance use.”
Over half of the Massachusetts overdoses involved someone with a diagnosed mental illness. Homelessness and a recent incarceration also raised the risk of a fatal overdose involving both opioids and stimulants.
"As a provider, these findings indicate a pressing need to address and treat not just opioid use disorder, but other substances that patients are misusing," said lead author Joshua Barocas, MD, an infectious disease physician at BMC. "To truly make a difference in reducing opioid overdose deaths, we must tackle issues such as homelessness and access to mental health services. This means not only investing in treatment but also implementing tailored programs that address the specific barriers to accessing care."
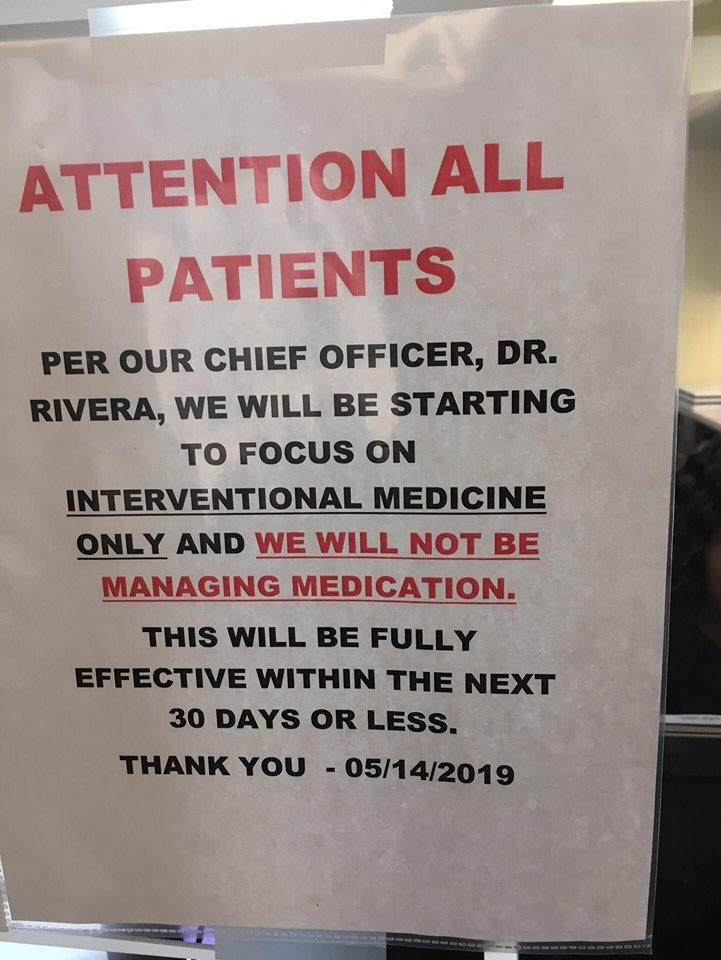
Opioid Prescriptions Down 39% since 2015
The number of opioid prescriptions has declined significantly in Massachusetts over the last four years, according to a recent report from the state’s Department of Public Health. In the first quarter of 2019 there were over 518,000 prescriptions filled for Schedule II opioids such as hydrocodone and oxycodone – a 39% decline from the first quarter of 2015.
But the decrease in prescriptions has failed to make much of a dent in Massachusetts’ opioid overdose rate, which peaked in 2016 with 2,100 deaths and remains stubbornly high.
SOURCE: MASSACHUSETTS DEPARTMENT OF PUBLIC HEALTH
In 2018, nearly nine out of ten opioid-related deaths (89%) in the state involved illicit fentanyl, with cocaine (39%), heroin (32%), and benzodiazepines (40%) such as Xanax also commonly found.
Only about ten percent of the overdose deaths in the fourth quarter of 2018 involved prescriptions opioids, virtually unchanged from the 2014-2015 study.