Widely Used Red Food Dye Linked to IBD
/By Pat Anson, PNN Editor
Allura Red is one of the most widely used artificial food dyes in the world. Also known as “Red Dye 40,” the dark red coloring is added to sodas, candies, breakfast cereals, condiments and dozens of other food products to make them more appetizing.
Over the years, Allura Red has been linked to a variety of different health conditions, including attention deficit hyperactivity disorder (ADHD) in children. Now there is emerging evidence that Allura Red may also trigger inflammatory bowel diseases (IBDs) such as Crohn’s and ulcerative colitis.
Researchers at McMaster University in Ontario, Canada exposed laboratory mice to Allura Red for 12 weeks — at about the same levels humans might consume — and found that it caused chronic inflammation in their gastrointestinal tracts and raised levels of serotonin, a hormone that affects mood and digestion.
“This study demonstrates significant harmful effects of Allura Red on gut health and identifies gut serotonin as a critical factor mediating these effects. These findings have important implication in the prevention and management of gut inflammation,” McMaster researcher Waliul Khan, PhD, said in a statement.
“What we have found is striking and alarming, as this common synthetic food dye is a possible dietary trigger for IBDs. This research is a significant advance in alerting the public on the potential harms of food dyes that we consume daily.”
Although Allura Red and eight other synthetic food dyes – all derived from petroleum -- are considered “safe for the general population” by the FDA, there have been relatively few studies of their effect on human health. Some experts believe the dyes disrupt the absorption of key minerals like zinc and iron, causing hyperactivity, allergic reactions and gut inflammation.
STRAWBERRY SODA CONTAINING ALLURA RED DYE
Recent research has helped establish the importance of gut health, and that bacteria can have profound effects – both harmful and beneficial -- on our immune and gastrointestinal systems. A 2022 study, for example, found evidence that a particular strain of bacteria causes abdominal pain, cramps, bloating, gas and diarrhea – symptoms common to IBD. A 2019 study linked gut bacteria to fibromyalgia.
Western diets that have a lot of processed food rich in fat, meat and sugar have also been linked to gut inflammation. Processed foods tend to have a lot of Allura Red and other chemical additives, and Khan believes they warrant further study.
“The literature suggests that the consumption of Allura Red also affects certain allergies, immune disorders and behavioural problems in children, such as attention deficit hyperactivity disorder,” said Khan, a professor of Pathology and Molecular Medicine at McMaster and principal investigator at the Farncombe Family Digestive Health Research Institute.
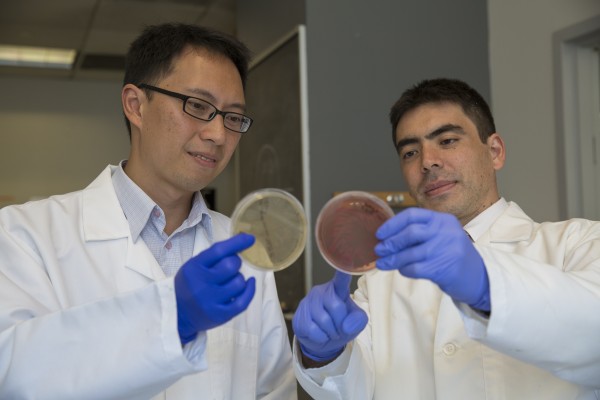
Khan and his colleagues published their findings in Nature Communications. Their study was funded by the Canadian Institutes of Health Research.