CDC: Still Not Enough Naloxone
/By Pat Anson, PNN Editor
The Trump Administration is stepping up efforts to increase prescribing of naloxone, an overdose recovery drug credited with saving thousands of lives.
Although naloxone prescriptions have increased dramatically, a new CDC Vital Signs report estimates that nearly 9 million additional prescriptions could have been dispensed last year if every patient with a high-dose opioid prescription was offered naloxone. Patients are considered “high risk” if they take an opioid dose of 50 morphine milligram equivalent (MME) or more per day.
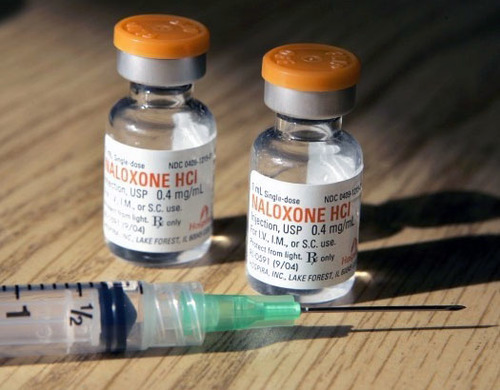
Naloxone has been used for years by first responders and emergency medical providers to revive overdose victims. Current efforts are focused on expanding access to the drug by prescribing it directly to patients considered at risk of an overdose.
In 2018, CDC researchers say only one naloxone prescription was dispensed for every 70 high-dose opioid prescriptions nationwide. Naloxone “under-prescribing” was even more acute in rural counties, which are nearly three times more likely to be ranked low in naloxone dispensing than metropolitan counties.
“It is clear from the data that there is still much needed education around the important role naloxone plays in reducing overdose deaths. The time is now to ensure all individuals who are prescribed high-dose opioids also receive naloxone as a potential life-saving intervention,” CDC Director Robert Redfield, MD, said in a statement.
Ironically, federal policies contribute to the under-prescribing. In 2018, most (71%) Medicare prescriptions for naloxone required a copay, compared to 42% for commercial insurance.
In January, the Food and Drug Administration encouraged drug makers to make naloxone available over-the-counter without a prescription. The FDA even developed an OTC label for Narcan, a naloxone nasal spray that sells for about $135. Seven months later, the FDA could not confirm to PNN that any company had submitted an application for an OTC version of naloxone.
Last year the Department of Health and Human Services released guidance urging doctors to “strongly consider” prescribing naloxone to patients on any dose of opioids when they also have respiratory conditions or obstructive sleep apnea, are co-prescribed benzodiazepines, have a mental health or substance abuse disorder, or a history of illegal drug use or prescription opioid misuse.
Many states are also taking steps to increase naloxone prescribing. California now requires doctors to “offer” naloxone prescriptions to pain patients deemed at high risk of an overdose. State law does not make the prescriptions mandatory, yet some patients say they were “blackmailed” by pharmacists who refused to fill their opioid scripts unless naloxone was also purchased. Patients around the country report similar experiences.
Unintended Consequences
The drumbeat for naloxone comes at a time when sales are already booming. There were 556,000 naloxone prescriptions in 2018, twice as many as in 2017.
There’s no doubt naloxone saves lives, but some researchers say the drug has had little effect on the overdose crisis and may in fact be making it worse. In a recent study published by SSRN, two economics professors warned of “unintended consequences” if naloxone becomes more widely available.
“We expect these unintended consequences to occur through two channels. First, the reduced risk of death makes opioid abuse more appealing, leading some to increase their opioid use — or use more potent forms of the drug — when they have naloxone as a safety net. Some of those abusers may become criminally active to fund their increased drug use,” wrote Jennifer Doleac, PhD, Texas A&M University, and co-author Anita Mukherjee, PhD, University of Wisconsin.
“Furthermore, expanding naloxone access might not in fact reduce mortality. Though the risk of death per opioid use falls, an increase in the number or potency of uses means the expected effect on mortality is ambiguous.”
The researchers said there were anecdotal reports of “naloxone parties” where attendees used heroin and prescription opioids to get high knowing they could be revived. News reports have also quoted first responders who are frustrated that the same opioid abusers “are saved again and again by naloxone without getting treatment.”