‘Zombie’ Nerve Cells Make Chronic Pain Worse
/By Pat Anson
The zombies are at it again.
Weeks after researchers announced a new way to treat low back pain by targeting so-called zombie cells – a new study suggests that peripheral nerve pain could also be treated with drugs that target aging cells.
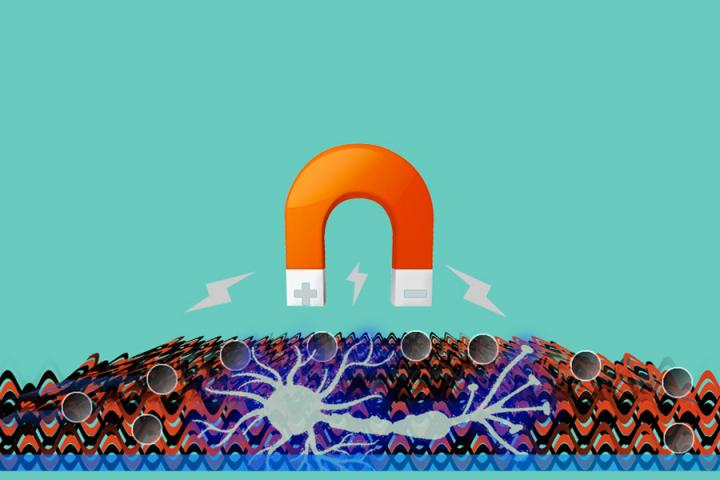
Senescent neurons are cells that stop dividing, but refuse to die and linger in the central nervous system. As people age, more and more of these “zombie cells” build up, secreting inflammatory agents that increase pain sensitivity and raise the risk of age-related diseases like arthritis, Alzheimer’s and Parkinson’s.
“Very little is known about underlying causes of pain experienced during aging. The prevalence of chronic pain in aging populations and the lack of effective and non-addictive treatments motivated this exploration into neuronal senescence as a potential mechanism,” Lauren Donovan, PhD, a research scientist at Stanford University, told PsyPost.
In studies on laboratory animals, Donovan and her colleagues at Stanford found that pain was amplified in older mice by senescent cells, which released inflammatory signals when the mice were injured. The same inflammatory reaction was found in younger mice, but was more pronounced in the older ones.
When the injured mice were treated with a drug called ABT263 – a compound that destroys senescent cells – the older mice showed less pain sensitivity and significant improvement in their weight-bearing behavior.
The younger mice treated with ABT263 showed only modest improvements in their pain-related behavior, which suggests that senescent cells play a significant role in causing chronic pain.
“The key takeaway for the average person is that as we age, some of our sensory neurons undergo a process called senescence, which may contribute to chronic pain,” said Donovan, who reported the findings in the journal Nature Neuroscience.
“In addition, we found that injury can exacerbate senescence in neurons, leading to an additive effect of aging and injury that may enhance pain. This research identifies a new potential target for treating chronic pain, especially in older individuals. It suggests that addressing cellular senescence in the nervous system can lead to new ways of managing pain and sensory dysfunction.”
Researchers at McGill University reported similar findings last month in studies on laboratory mice with damaged discs. When the mice were given drugs that targeted senescent cells in their spines, they experienced less pain and their bone quality improved.
Previous animal studies have shown that senolytic drugs can reverse osteoarthritis by eliminating senescent cells, giving the body a chance to repair and rejuvenate damaged cartilage.
The findings need to be replicated in humans, but they suggest that senolytic drugs that target zombie cells have the potential to prevent or even cure some age-related diseases.