Study Finds Why Some Patients Do Poorly with Spinal Cord Stimulators
/By Pat Anson, PNN Editor
Spinal cord stimulators (SCSs) are often considered the treatment of last resort for people with severe back or leg pain, who don’t respond well to more conventional ways of treating pain.
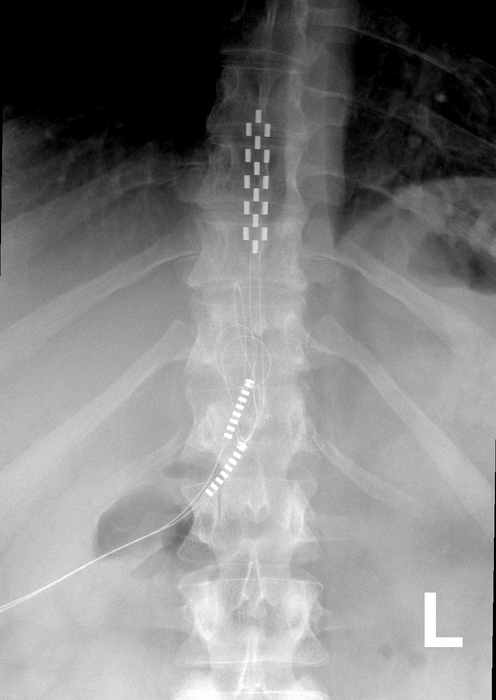
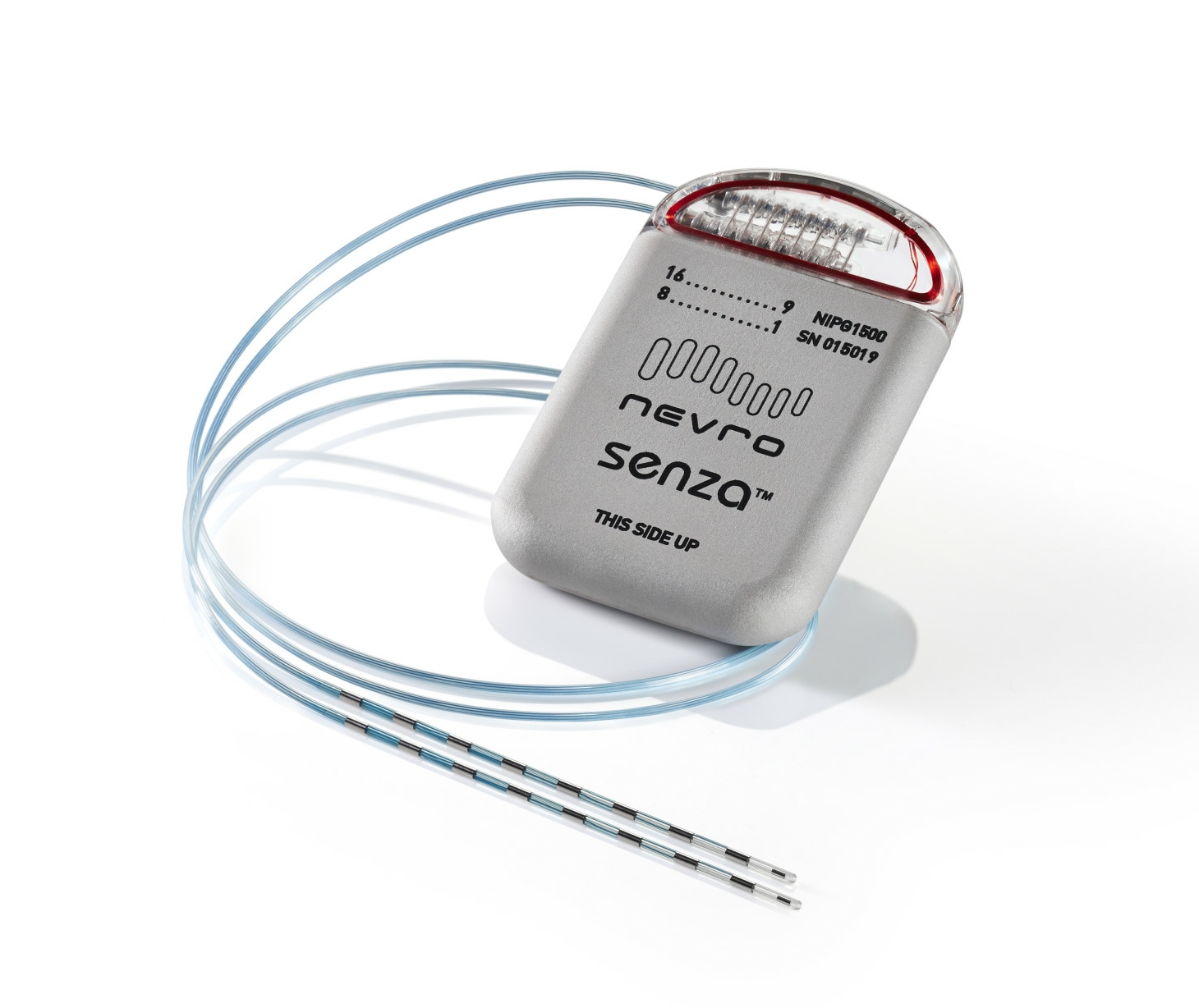
The neuromodulation devices are surgically placed near the spine and send out mild electrical impulses to mask pain signals. Because stimulators are invasive and have poor success rates, it’s customary for patients to go through a short trial period before having the devices surgically implanted.
A new study has documented why some patients do well with stimulators and others don’t.
In a retrospective analysis, researchers at the University of Kansas Medical Center looked at 237 patients who received SCSs, about a third of them considered “nonresponders.” They found that people with severe pain and disability who fear physical activity because of the pain it might cause – a condition known as kinesiophobia – are significantly less likely to respond to the devices.
The study is being presented this month at the annual meeting of the American Society of Regional Anesthesia and Pain Medicine (ASRA).
Researchers analyzed several patient characteristics, such as their age, gender, body mass index, history of spinal surgery, diabetes, alcohol and tobacco use, psychiatric illness, and use of opioids. None appeared to have an association with how a patient responds to SCS.
But researchers found that three out of four (76%) nonresponders had clinically high levels of kinesiophobia, compared to about half (56%) of those who did respond to SCS treatment. Nonresponders were also more likely to have severe pain, disability, and to complain or worry about their pain – a condition known as “catastrophizing.”
“Collectively, our findings indicate a clinically relevant association of high levels of kinesiophobia, greater disability, severe pain intensity and pain catastrophizing, as subtle indicators, and possible predictive factors to nonresponders,” researchers said.
“As such, it may be appropriate to utilize preoperative screening tools for these factors to help optimize patient selection and predict a patient’s response to neuromodulation. Furthermore, if risk factors are present, it might be prudent to consider a pre-rehabilitation program with pain neuroscience patient education prior to SCS therapy to address these modifiable risk factors and potentially enhance outcomes in neuromodulation.”
About 50,000 spinal cord stimulators are implanted annually in the U.S. The devices are often touted as a safer alternative to opioid pain medication, although a growing number of studies have questioned their safety and efficacy.
A recent Cochrane review of SCSs concluded the devices work no better than a placebo for treating chronic low back pain, and provide little to no benefit in improving quality of life. That negative review led some doctors who perform the surgeries to demand a retraction from Cochrane because of “striking errors in the methodology, execution and conclusions” of the study.
Meanwhile, a 2018 investigation found that SCSs have some of the worst safety records of medical devices and called for better FDA oversight of their growing use in pain management. A subsequent FDA review of complaints involving stimulators found that nearly a third were reports of unsatisfactory pain relief.
Yet another recent study found that many patients given stimulators did not reduce their use of opioids, and continued getting procedures such as epidurals, corticosteroid injections and radiofrequency ablation to relieve their pain.