An Old Disease Returns in Modern Times
/By Pat Anson, PNN Editor
Dr. Forest Tennant may no longer be practicing medicine, but he continues his groundbreaking research into the causes and treatment of adhesive arachnoiditis (AA), a chronic, progressive and painful inflammation of spinal nerves.
Once a rare disease linked in the 19th century to infections such as syphilis and tuberculosis, arachnoiditis is re-appearing in surprising numbers and for completely different reasons. Tennant believes millions of Americans may have developed AA, which is often misdiagnosed as “failed back syndrome” – chronic back pain that fails to respond or grows worse after invasive spinal procedures.
“I think it’s now the number one cause of really severe pain in the country. I don’t think there’s any question about that,” says Tennant. “When I closed my clinic, about 70% of the people in there who had to take high dose opioids had an issue with arachnoiditis.”
Tennant and co-author Ingrid Hollis have written a new book -- “Adhesive Arachnoiditis: An Old Disease Re-Emerges in Modern Times” -- to help doctors and patients recognize the symptoms of AA and to offer hope for treating a disease long thought to be incurable.
Why is AA re-emerging? Tennant says a “perfect storm” began to appear around the year 2000, when longer lifespans, obesity and sedentary lifestyles contributed to more cases. Lack of exercise has long been associated with chronic back pain.
Arthritis, accidents, repetitive stress injuries and even Lyme disease can also cause degenerative spinal conditions that lead to AA.
“But the real factor contributing is probably sedentary lifestyles. Look at the number of people spending 6 to 8 hours a day in front of a computer or TV screen,” says Tennant. “I’m really trying to bring attention to the fact that people need to be aware that this is something that can happen because of our lifestyles.”
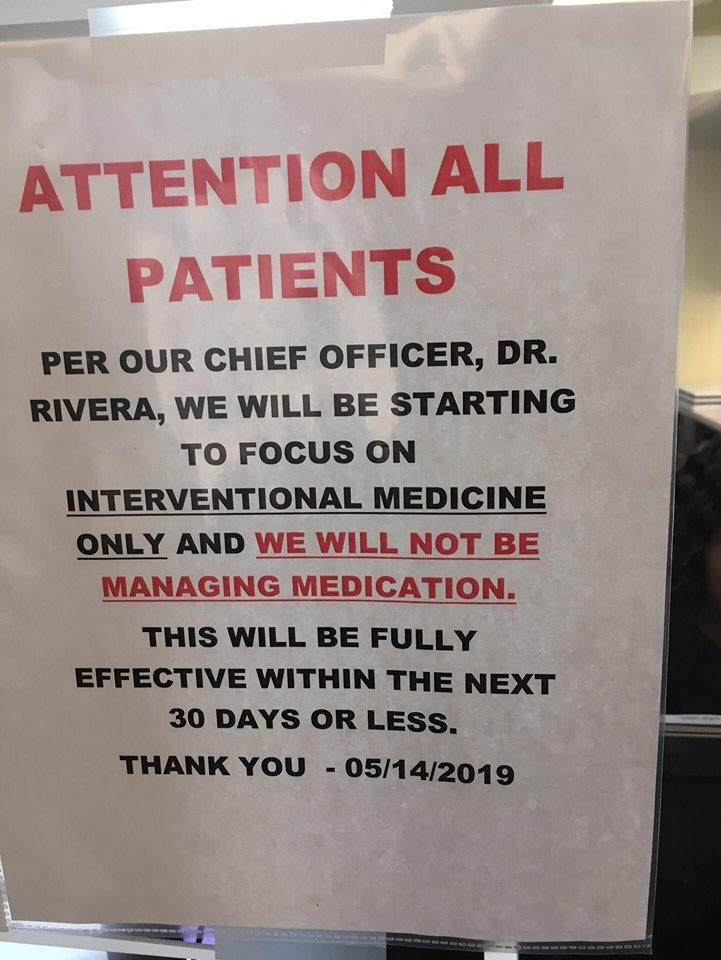
As more Americans sought treatment for back pain, millions were given “interventional” procedures such as epidural steroid injections and spinal surgeries – a trend that appears to have increased as opioids fell out of favor. While most interventional procedures do not result in complications, all it takes is a single misplaced needle or scalpel to damage the spinal cord and trigger a lifetime sentence of AA.
“Everybody wants to blame the epidurals and the surgeries for these problems, but they were only doing these things when there were medical indications for them. And if they do the surgeries and the epidurals, a certain percentage of them are going to get arachnoiditis,” Tennant told PNN.
“There is a risk/benefit to these procedures. If you start going in and operating on the spine or you have half a dozen epidural injections, you start increasing your risk for developing adhesive arachnoiditis. One of the points I want to make is that it is the underlining spinal conditions that are causing the problems. The interventions and the surgeries may accelerate it, but the condition was already set.”
For many years, Tennant was one of the few doctors in the U.S. willing to treat AA patients with high doses of opioids. Intractable pain patients from around the country traveled to California to see Tennant – which led to his home and office being raided by the DEA in 2017. No charges were ever filed against Tennant, but the stress of being investigated led to his retirement from clinical practice.
Tennant now consults with other doctors and is developing new protocols for treating AA with hormones and drugs that reduce pain and inflammation while stimulating nerve growth. His book includes a self-screening test for patients and a list of AA symptoms.
Most essential in any AA diagnosis is a good MRI of the spine. Tennant has a library of over 300 MRI’s sent to him by patients and doctors in dozens of countries — a testament to how AA is re-emerging worldwide.
(Dr. Tennant and the Tennant Foundation have given financial support to Pain News Network and are currently sponsoring PNN’s Patient Resources section.)