Virtual Reality Has Long-Term Benefits for Patients with Back Pain
/By Pat Anson, PNN Editor
A novel treatment that combines virtual reality with cognitive behavioral therapy significantly reduced pain levels and other symptoms in patients with chronic back or neck pain, according to results of a new study presented at the annual meeting of the Congress of Neurological Surgeons.
Unlike other therapies using virtual reality (VR) – which temporarily distract people from their pain – patients in this study had long term reductions in their pain, anxiety and depression. This suggests that combining VR with cognitive behavioral therapy (CBT) induces neuroplasticity, a “rewiring” of the brain and nervous system that reduces the impact of physical and emotional trauma.
“What we found is it actually creates new neural pathways to form, what's called neuroplastic reprogramming or neuroplastic change, and that actually creates a more resilient patient,” said co-author Gerry Stanley, MD, Chief Medical Officer of Harvard MedTech, a medical device company that offers VR therapy.
“The patient who may be thinking about their pain 22 hours a day, and their pain (level) has always been eight or nine, now thinks about their pain one or two hours a day and their pain (level) is a three or four, because the brain is no longer fixating on it. So it allows for, I don't want to say permanent distraction, it’s really neuroplastic reprogramming.”
Stanley and his colleagues enrolled 145 patients with non-operative degenerative neck or back pain in Harvard MedTech’s Vx Therapy program, which included daily virtual reality sessions for 14 weeks and weekly telephone calls with a therapist trained in CBT.
Unlike other VR therapies, which encourage physical activity, participants sat stationary in a chair while watching and listening to prerecorded programs with a headset and earphones. The VR programs come in four categories that emphasize education, meditation, distraction or entertainment, depending on the patient’s needs and goals.
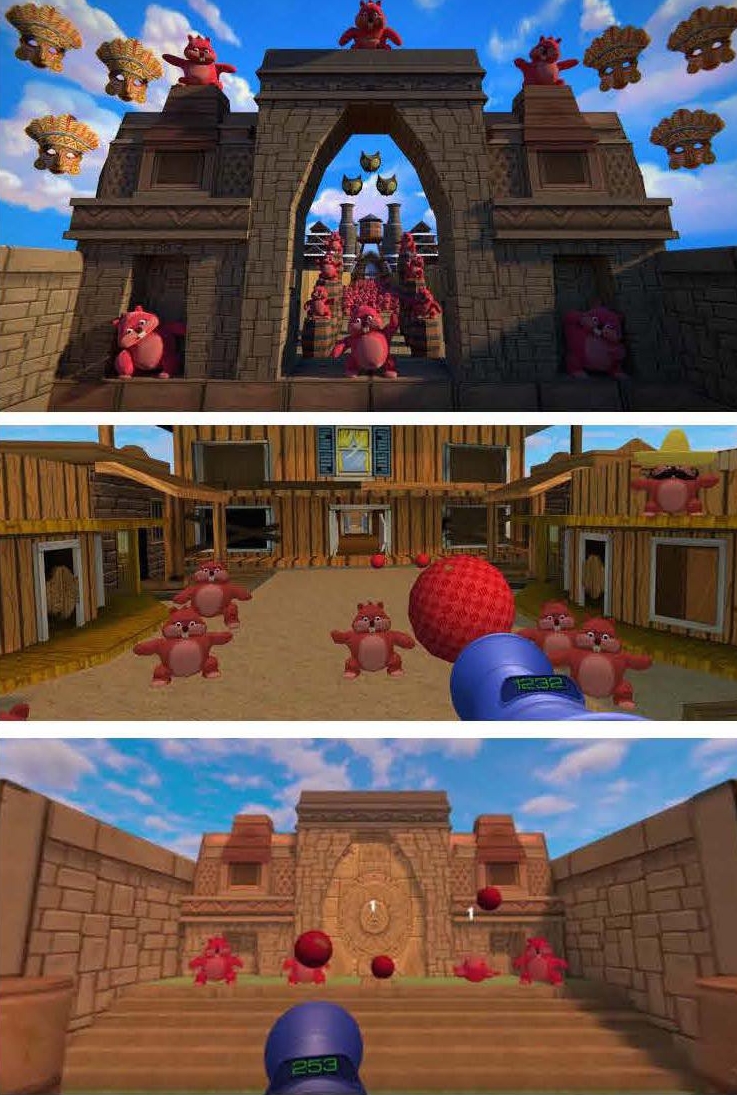
HARVARD MEDTECH IMAGE
After 14 weeks, results showed that Vx Therapy reduced pain and anxiety during sessions by an average of 33% and 46%, respectively. The duration of pain relief also increased over time, from 2.5 hours in the first weeks of treatment to 4.5 hours in the final weeks.
The study has not been peer-reviewed or published yet, but Stanley says the findings mirror what his company has learned after treating about 4,000 patients. The benefits of Vx Therapy continue long after the treatment ends, with many patients still reporting improvement after two years.
“They're often reporting the same level of resiliency. I think a lot of it is they start getting into better sleep patterns,” he told PNN. “And they really get good at meditation. Most people fail in meditation because of distractions. But when they're doing it in the virtual reality, they get very good at it. So they really develop some nice, I'm going to say muscle memory, even though I know it's cognitive. But they do develop a little bit of muscle memory around the meditation.”
Because Vx Therapy is done remotely, it’s available to any patient regardless of location, as long as they have a prescription. Some worker compensation insurers cover the treatment.
Previous studies have also suggested that virtual reality therapy has long-term benefits for people with chronic back pain. A 2022 study showed that people with moderate lower back pain reported improvements in pain, function, mood and sleep six months after treatment ended.