Study: Virtual Reality Can Relieve Severe Chronic Pain
/By Pat Anson, PNN Editor
Therapeutic virtual reality (VR) may finally be on the verge of going mainstream. For the first time, research has shown that VR can help relieve a variety of pain conditions and is most effective for severe chronic pain.
"I believe that one day soon VR will be part of every doctor's tool kit for pain management," says Brennan Spiegel, MD, director of Health Service Research at Cedars-Sinai Medical Center in Los Angeles.
Spiegel is lead author of a new study published in PLOS ONE, which looked at the effectiveness of VR in 120 hospitalized adult patients suffering from neurological, orthopedic, gastrointestinal or cancer pain. All of the patients were being treated with opioid medication and had a pain score of at least three on a 1 to 10 pain scale.
“There’s been decades of research testing VR in highly controlled environments — university laboratories, the psychology department and so on,” Brennan told MobiHealthNews. “This study is really letting VR free and seeing what happens. What I mean by that is it’s a pragmatic study where we didn’t want to control every single element of the study, but literally just see [what would happen] if we were to give it to a broad range of people in the hospital with pain; how would it do compared to a control condition already available in the hospital?”
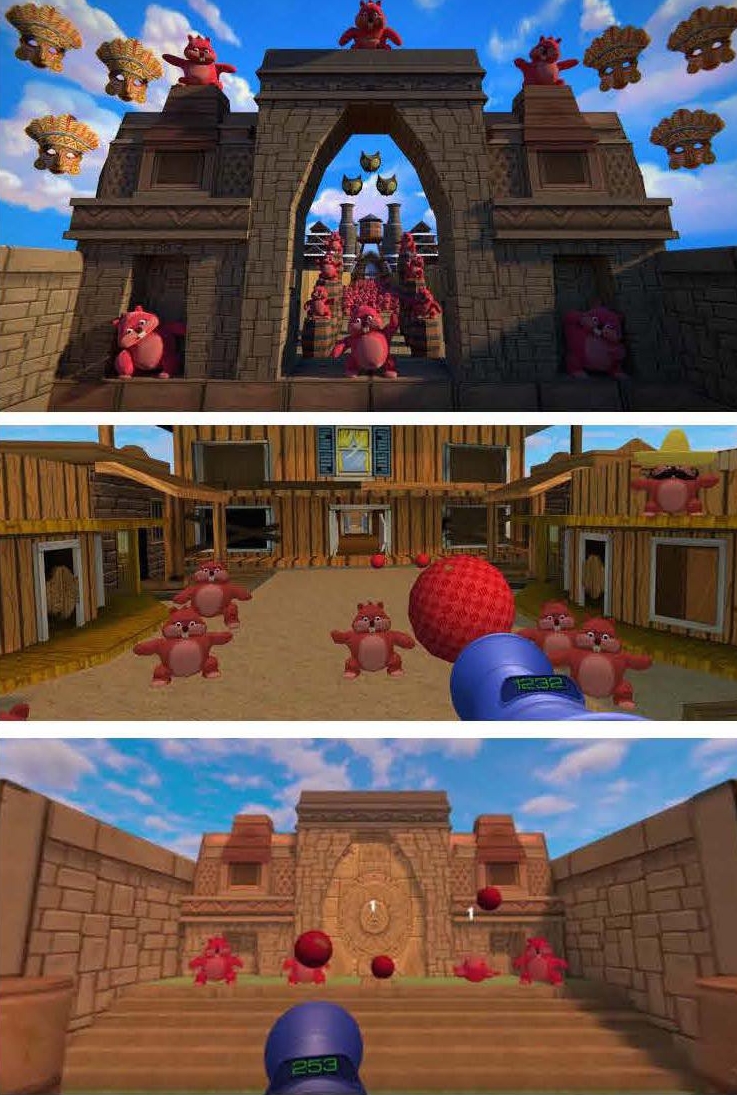
Half of the patients were given VR goggles with a variety of relaxing and meditative experiences to choose from. They were advised to use the headsets three times a day for 10 minutes — and as needed for breakthrough pain – for three days.
The other participants were instructed to tune their hospital room TVs to a health and wellness channel that offered programs on guided-relaxation, yoga and meditation.
Several times a day, nurses asked all the patients to rate their pain on the pain scale.
The study found that on-demand use of VR resulted in a small but statistically significant improvement in pain scores compared to the TV group, with patients in the VR group averaging 1.7 points lower on the pain scale. VR patients with the most severe baseline pain of 7 or more reduced their pain scores three points lower than the TV group.
"This is our largest and most ambitious VR study to date," Spiegel said. "Our results support previous research that VR can meaningfully reduce pain using a nonaddictive, drug-free treatment for people experience a range of different pain conditions."
In the previous study, patients who watched a 15-minute nature video had a 13% drop in their pain scores, while patients who played an animated game had a 24% decline.
Spiegel says the current study showed that VR can do more than just distract the mind from pain, but may even block pain signals from reaching the brain by overwhelming the brain with visual and audio stimulation.
Several patients found VR so helpful in managing their pain that they now use it regularly at home. One of them is 70-year old Joseph Norris, a retired Air Force lieutenant colonel, who suffers from chronic pain in his spine, back and hips. Norris started using VR six months ago, and today uses his VR headset once a week to help relax and distract.
"VR is a tool I use to successfully divert attention away from my pain, and it helps me reinforce my breathing pattern," he said.
There remains a great deal of skepticism about VR, particularly among older patients. Spiegel and his colleagues evaluated nearly 600 patients for the study, but many chose not to participate.
“Patients expressed varying degrees of skepticism, fear, sense of vulnerability, concern regarding psychological consequences, or simply not wanting to be bothered by using the equipment. We believe it is important for the digital health community to recognize that despite the great promise of health technology, clinical realities can undermine expectations,” he wrote.
Spiegel and his research team are currently involved in a study following patients using VR in their homes for 60 days.