7-OH Is a Breakthrough for Pain Relief and Should Remain Legal
/By Crystal Lindell
This week, Missouri took a step towards banning most 7-OH products, joining a long list of governmental bodies considering similar things.
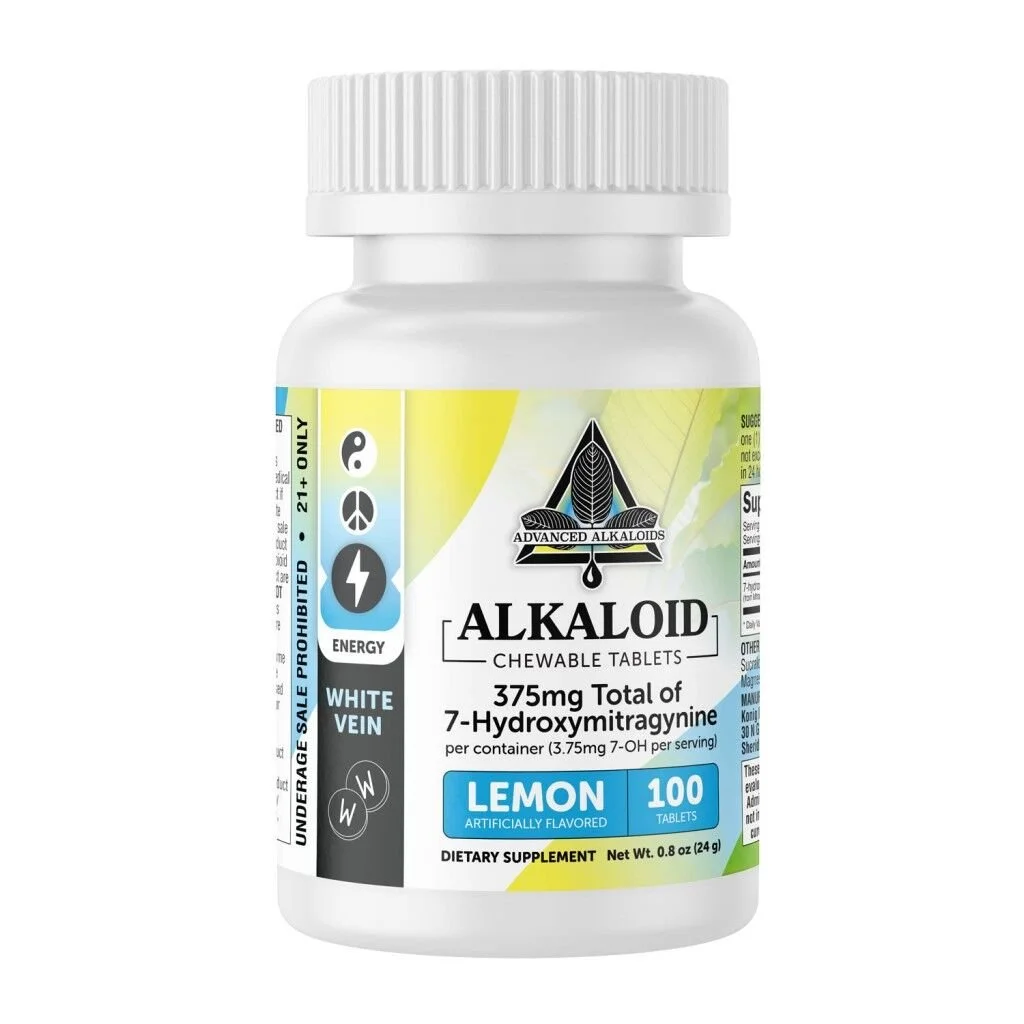
If you’re unfamiliar, 7-OH is an alkaloid that occurs naturally in kratom, the full name of which is 7-hydroxymitragynine. When concentrated, it has opioid-like effects that can relieve pain and boost energy levels.
The interesting part is that 7-OH doesn’t cause respiratory depression the way opioids do, which means it is not deadly the way opioids can be.
Unfortunately, multiple governmental bodies are attempting to ban it. While the FDA would like to ban it nationwide, states like Florida, Ohio and Kentucky have already banned it, while health officials in California are taking it off store shelves.
The Missouri Senate is considering a bill that would also effectively ban 7-OH. The proposed law would prohibit the sale of all kratom products to people under the age of 21 and specifically limit the 7-OH content in products to 2%.
Since many contain about 50% 7-OH or even more, that would essentially prohibit the sale of all 7-OH products. Violators could face felony charges if the bill becomes law.
The Missouri Independent reported that during a committee hearing on the bill, State Sen. Maggie Nurrenbern (D) of Kansas City said several families submitted statements calling 7-OH products “highly addictive, unregulated drugs” that have impacted their loved ones and children.
“I don’t know if there’s any more pressing issue before us than making sure that kids don’t have access to these drugs,” Nurrenbern told the committee. “As well as making sure that we’re not doing further damage to our community right now that’s already grappling with so much in terms of addiction and mental health.”
A Painkiller That Actually Works
It’s disheartening to see 7-OH framed this way, when I know just how much value it has for the lives of the millions of people suffering from chronic pain.
For years, we’ve been told that the reason opioid prescriptions had to be greatly restricted was because of overdose deaths. But now that we finally have something that actually treats pain without directly causing OD deaths, officials are still trying to claim it is doing “damage” to the community.
What about the damage caused by chronic pain?
My life is littered with hellish stories about people I know who couldn’t get pain meds when they needed them. In fact, comment sections on PNN’s social media are often overflowing with the same type of stories.
Readers tell us many doctors dismiss their pain, refuse to prescribe opioid medication, and leave patients to suffer. Some pharmacists also refuse to fill opioid prescriptions and get irate when pushed.
I have even seen numerous patients lamenting that they have lost the will to live because their severe pain is untreated. I have been there myself. Before I found my current doctor — who prescribes me enough pain medication to function — I still remember talking to my mom about how, if I do kill myself, I want her to understand that death would be a mercy for me.
But now there is an over the counter substance that actually treats pain, and I just have to call it what it feels like to me as a patient: a miracle.
In fact, I would argue that 7-OH is likely the closest we will come in my lifetime to seeing something like hydrocodone being sold OTC – something I have long advocated for.
In a humane society, everyone should have access to effective pain treatment, especially in a country without universal healthcare or insurance coverage.
I was talking to my fiancé about a surgery he had a few years ago, where the operating surgeon initially refused to give him opioid medication for post-operative pain. The doctor claimed that his other patients had only needed ibuprofen — after he took a scalpel and sliced open their arms to repair a nerve.
While my partner was still coming out of anesthesia, I had to argue with his surgeon to make sure he was sent home with at least a handful of Norco.
I had made the mistake in the past of not doing this after my partner’s nose surgery, and then I was left to watch him suffer on the couch for three days while he lamented that every time he tried to breathe, it felt like death.
If either situation happened today, we could save ourselves from so much stress and agony because he could just take 7-OH post-op. Yes, 7-OH is that good of a painkiller.
If doctors were smart they would be jumping all over 7-OH. Finally, something that actually relieves pain and doesn’t kill their patients. It’s what we have all been looking for!
But no, doctors are not recommending 7-OH. In fact, most have never heard of it, while state and local governments either ban it or threaten to do so.
Yes, there are some downsides. The main one is how expensive it is. One 7-OH chewable tablet, which has 4 servings, will run you around $10.
It can also be difficult to figure out which brand works best for you, in large part because there’s so little regulation of kratom or 7-OH, making it difficult to know what each brand puts into their tablets and how much is in there.
My circle of people really like using the brand 7Stax, but you can also browse through the r/7_hydroxymitragynine subreddit for additional recommendations and user experiences.
You should know that 7-OH can cause dependence and withdrawal symptoms if you abruptly stop taking it. As someone who has used opioids for over a decade to manage pain, I am an expert on tapering down medications to avoid withdrawal. Newcomers may have some trial and error time before they figure out what’s best for their own bodies.
There’s also not much research on how 7-OH interacts with other drugs or health conditions, not to mention the lack of information about long-term side effects.
That is largely why I am still hesitant to recommend it to elderly relatives, as their health tends to be more fragile. Although, paradoxically, they also tend to be much more likely to have chronic pain.
With everything going on in the news, it does seem like the fight to make 7-OH illegal has taken a backseat to other issues.
What I would say is that if you have been hesitant to try 7-OH because you don’t want to waste money on another supplement that probably won’t work, then I can vouch for the fact that it does work on my pain.
I’m not a doctor, just a patient who also has a lot of loved ones with chronic pain. And I can tell you that everyone I know who tries 7-OH finds it to be effective.
If you are among those who have already found 7-OH to be effective, I encourage you to be proactive by reaching out to your local government officials to tell them how important it is for you. I would also encourage you to make yourself available to local reporters when possible, so that they can offer more balanced coverage of what 7-OH is and what it does.
While 7-OH is a breakthrough, it will only stay that way if it remains legal. We all have to fight to keep it that way.