How to End the ‘Opioid Paradox’
/By Pat Anson, PNN Editor
Three public health and pain management experts are calling for a major shift in strategy to combat the U.S. opioid crisis, one that doesn’t just focus on pill counts and punishing doctors deemed to be “overprescribing” opioids.
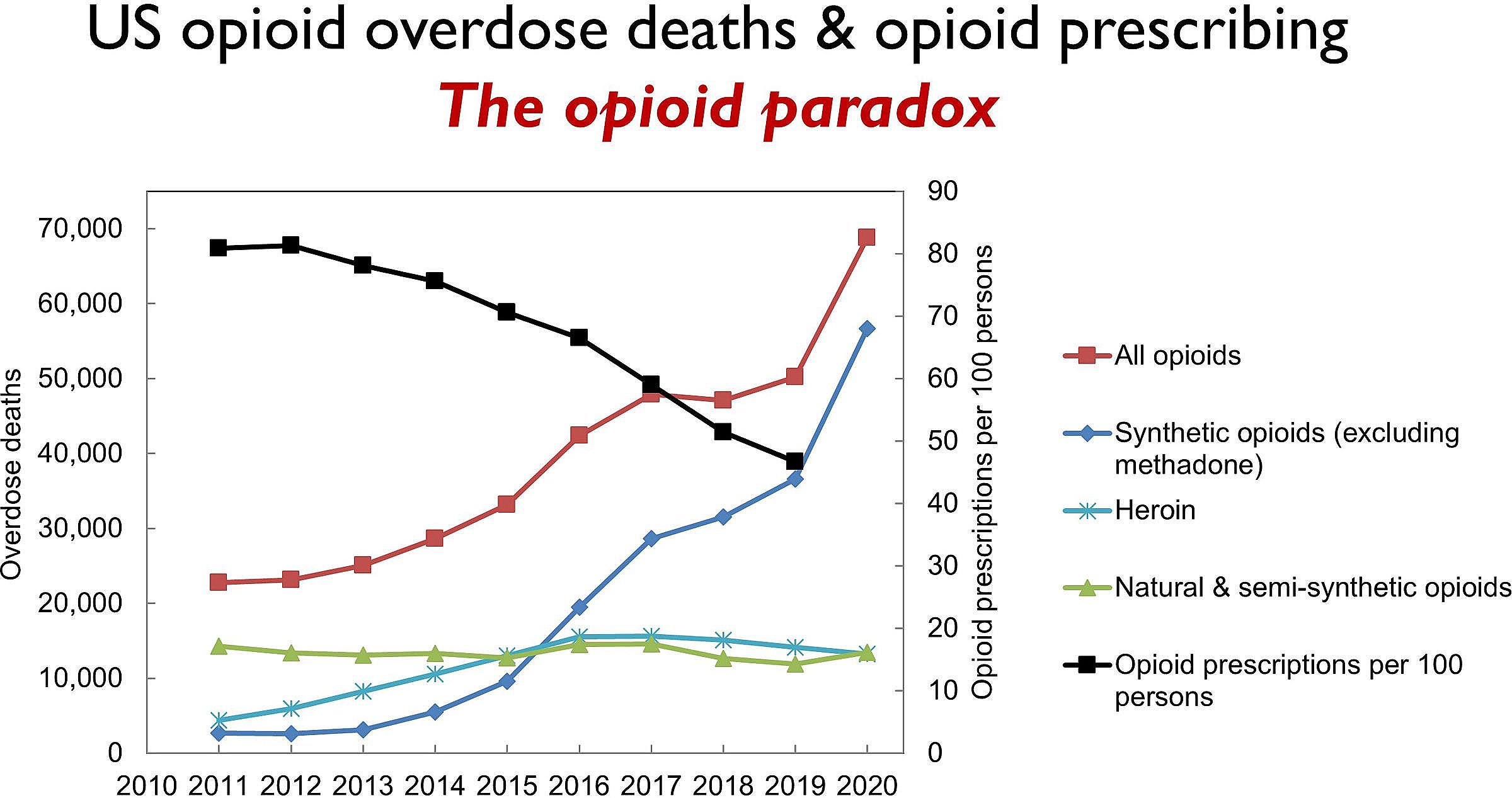
In an op/ed recently published online in Anesthesiology, the official journal of the American Society of Anesthesiologists, Editor-in-Chief Evan Kharasch, MD, Editor J. David Clark, MD, and former U.S. Surgeon General Jerome Adams, MD, said current policies are failing to address what they call the “opioid paradox” --- how opioid overdose deaths have risen to record levels even as opioid prescribing has fallen to 20-year lows.
SOURCE: ANESTHESIOLOGY
“Overall, the nation’s response to the oral opioid crisis has been to tighten patient supplies and impose institutional and practitioner quality indicators based on pill counts. Governments, payers, and pharmacies have assumed authority for limiting opioid prescribing, often in indiscriminate ways, based on misinterpretation of Centers for Disease Control guidelines or based on no real guidance at all,” they wrote.
“Pill counts have become de facto standards employed by healthcare organizations to highlight their success in reducing opioid use, yet there is no discussion of how those reductions are affecting patient outcomes. One crucial problem is that agencies mandating policy restrictions do not measure, nor are they accountable for, patient outcomes. Mandated opioid prescribing limits may be too low to adequately control pain, or too high to reduce oversupply.”
The three authors say more novel and comprehensive approaches are needed to better manage the supply of prescription opioids, prevent diversion and address the opioid paradox.
“It involves immediate action to address opioid use, storage, return, and harm reduction, with a specific focus on patients and communities,” they explained.
Reduce Demand
In recent years, federal and state agencies, healthcare organizations and insurers have created new guidelines for treating pain – many of which take a one-size-fits-all approach to opioid prescribing that doesn’t take into account an individual patient’s needs.
“Legislative, regulatory, and insurer limitations on opioid prescribing alone have not met their intended goals and are considered unlikely to achieve them. One reason is that they impose tight restrictions on an extremely heterogeneous patient population,” the authors said.
Rather than limiting or withholding opioids after surgery – which has become increasingly common -- Drs. Kharasch, Clark and Adams urge anesthesiologists and surgeons to provide patients with enough opioids for adequate pain relief, because undertreated acute pain can turn into chronic pain and become a risk factor for opioid misuse.
Smaller opioid doses may be effective in treating postoperative pain, the authors said, if they are combined with multimodal strategies that also employ non-opioid medications and therapies. So too may the use of longer-acting opioids such as methadone, which can result in less postoperative pain and relief that lasts for weeks or months after a single dose.
Proper Disposal of Leftover Pills
Hundreds of millions of opioid pills are dispensed to patients but go unused each year, according to the authors. Most leftover pills are kept by patients and few are safely stored. Only a fraction are disposed of properly or returned.
"The current difficulty of returning prescription opioids contrasts markedly with the ease of obtaining them. This is illogical and unsafe," Drs. Kharasch, Clark and Adams said.
They believe pharmacies that dispense opioids should be required to provide patients with instructions for proper return and disposal; the addresses and telephone numbers of disposal stations; and a pre-addressed, prepaid envelope for returning unused pills. Disposal stations should be available year-round, not just on “Prescription Drug Take Back” days.
Another novel approach would be opioid “buy-back” programs, similar to the gun buy-backs used by law enforcement agencies to get unneeded firearms off the street. One pilot compensation program for opioids found that 30% of surgery patients were willing to participate in buy-backs, selling their leftover opioids for up to $50.
Partial Fills
Kharasch, Clark and Adams also suggest more partial filling of opioid prescriptions. A 2016 federal law allows both patients and clinicians to request partial filling of prescriptions for hydrocodone, oxycodone and other strong Schedule II opioids. Partial filling for schedule III–V weaker opioids has been permitted for decades, but is not widely practiced.
According to one estimate, 36 million postoperative opioid prescriptions could be partially filled each year. One hurdle for partial fills is the extra paperwork and cost to pharmacies, estimated at $15 for each prescription.
“Partial opioid fills could be the single most effective intervention to deplete America’s medicine cabinets of unused prescription opioid pills, shrink the opioid pool, improve the prescription opioid ecosystem, and prevent misuse, diversion, and death,” the authors said.
Kharasch, Clark and Adams place an emphasis on reducing diversion, even though less than one percent of legally prescribed opioids are diverted, according to the DEA. Partial fills may reduce leftover pills in medicine cabinets, but they won’t do anything to prevent the wholesale theft of opioids from hospitals, pharmacies and the pharmaceutical supply chain.
The authors also buy into the myth that most street drug users start with prescription opioids, and that pain patients denied opioids “switch to illicit drugs” and fentanyl-laced counterfeit pills.
But Kharasch, Clark and Adams do have some interesting ideas about addressing the opioid paradox – chief among them the long overdue recognition that current opioid reduction strategies have been a complete failure.
“Attempts to solve the problem by restricting patient supply alone have not succeeded, and the prescription opioid pool remains large. Additional novel efforts to shrink the pool are needed, both by diminishing demand (reducing pain through better treatment) and by facilitating opioid disposal and return,” they concluded.