Will Cannabis Change the Candy Industry?
/By Crystal Lindell, PNN Columnist
A bag of Heady Harvest CBD Gummies sold by CBD Genesis doesn’t look that much different than any other bag of gummies in the candy aisle — sleek packaging, a clear front panel to show the product and a well-designed logo. And you can find bags just like them hanging right there on the shelf in many gas stations, not too far from the energy drinks and lottery tickets.
It’s exactly the type of packaging that’s making CBD go mainstream. In fact, the only thing that makes them any different than a regular bag of gummies is the price — $24.99 for just 20 bears.
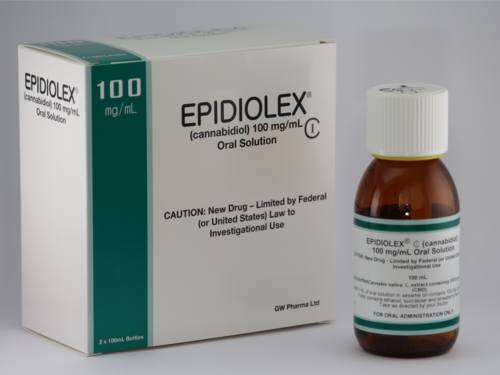
CBD, which stands for cannabidiol, is a compound found in marijuana plants, and the product is typically sold over the counter in the form of drops, candy and other products.
“The natural compound, called cannabidiol, is one of more than 100 cannabinoids found in the cannabis plant,” says BDS Analytics. “On its own it won’t get people high. But researchers are finding more and more medical applications for CBD, and consumers and companies increasingly are exploring the compound.”
The firm says that while the broad marijuana edibles category grew by 36 percent for much of last year in Colorado, Oregon and Washington, high-CBD edibles expanded by 110 percent.
And high-CBD chocolates reached 217 percent growth on $11.45 million in sales, while high-CBD candy grew by 169.5 percent last year, compared to 51 percent for candy in general, according to BDS.
Legally, it's still very much a gray area, though.
According to recent article in the Wall Street Journal, “DEA spokesman Melvin Patterson says CBD-containing product appearing on shelves ‘is there illegally,’ but enforcement is not a priority for the agency, which is focused on the opioid crisis. In the states that have legalized cannabis use, ‘DEA is not after that. That would take a lot of manpower that DEA doesn’t have,’ he says.”
And with the product being sold over the counter in many places, it can be confusing for consumers who think they’re buying something that’s totally above board.
It’s that kind of murky gray area that understandably makes it hard for more mainstream candy companies to get involved in the market. But as the products grow in popularity, it’s hard to ignore their potential financial impact.
It’s not that crazy to picture a day when Hershey, Mars or other major manufacturers are launching their own lines of CBD candy. How long that takes may only depend on how long for-profit companies want to ignore what is clearly becoming a for-profit market segment.
This article originally appeared in Candy Industry and is republished with permission.
Crystal Lindell is a journalist who lives in Illinois. She eats too much Taco Bell, drinks too much espresso, and spends too much time looking for the perfect pink lipstick. Crystal has hypermobile Ehlers-Danlos syndrome.
Crystal writes about it on her blog, “The Only Certainty is Bad Grammar.”
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represent the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.