The High Cost of Anxiety Drugs Gives Me Anxiety
/By Crystal Lindell, Columnist
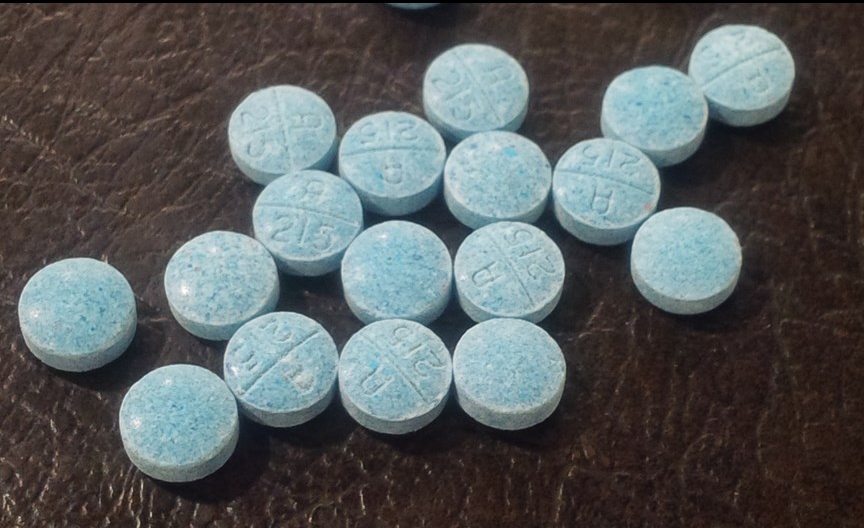
I recently got a new prescription for a drug that’s supposed to help with my anxiety — which is a debilitating mix caused by opioid withdrawal and what I would call a base level of anxiety that runs through my bones.
The ironic thing about what happened is that when I went to pick up the anxiety medication, the cost of the prescription nearly gave me an anxiety attack — right there at the pharmacy.
The co-pay was $65.
It gets worse. My doctor wanted to gradually move me up on the dose, so he had ordered some 10 mg pills and some 20 mg pills. The insurance company wanted me to pay $65 for EACH dose! That’s $130.
We need to talk about co-pays. There’s this misconception in America that if you have health insurance, then you don’t have to really worry about medical bills.
But that’s so incredibly not true.
Listen, I wish a $65 co-pay for medication was no big deal for me. I wish I could just whip out some hundos every time I stopped in the pharmacy and throw them around like confetti, but alas, I am not a rapper or a Kardashian.
So when my insurance company tells me that the medication I am taking is “not preferred” and thus comes with a $65 co-pay, I cry a little inside. Especially since it’s a monthly prescription.
Add in a couple other meds ($25/month) and I’m looking at $90 a month for prescriptions. That’s literally an electric bill, or four tanks of gas, or about 10 percent of my rent.
I asked the insurance company if I could appeal the fact that it’s not their preferred medication, seeing as how I had what I thought were very valid reasons.
1) I had a horrific reaction to the one that is preferred, and ended up in the ER.
2) As a response to the horrific reaction to the other drug, my doctor ran genetic testing to see which meds would work best for me, and after a lot of consideration we decided on this one.
3) This is the medication my doctor chose.
But the insurance company was basically like, “Umm, yeah, no you can’t appeal.” Something about how they do technically cover it, so there’s nothing to appeal.
They literally tried to tell me that my doctor should just prescribe one of the preferred meds, completely ignoring the fact that my psychiatrist had literally spent hours with me talking about all the pros and cons before he decided on this one.
And then they had the audacity to act like it was no big deal. But if it’s no big deal, why don’t they pay the $65 then?
My $65 co-pay is just one small example of all the ways people with insurance can still find themselves with mountains of medical bills. There’s also the $30 co-pay for every single doctor’s appointment, and the $2,500 deductibles you run into every time you’re in the ER.
I live paycheck to paycheck, and all the medicals bills can make it hard to breathe. In fact, it’s enough to give a girl an anxiety attack.
Crystal Lindell is a journalist who lives in Illinois. She loves Taco Bell, watching "Burn Notice" episodes on Netflix and Snicker's Bites. She has had intercostal neuralgia since February 2013.
Crystal writes about it on her blog, “The Only Certainty is Bad Grammar.”
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represent the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.