Walgreens Joins CVS in Fighting DOJ Opioid Lawsuits
/By Crystal Lindel
Walgreens is fighting back against a new Department of Justice lawsuit, using a tactic that mirrors CVS’s public response to a similar DOJ lawsuit filed last month.
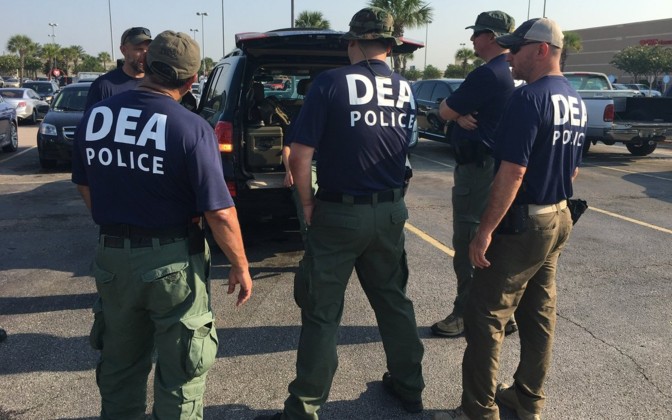
In both lawsuits, the DOJ claims that Walgreens and CVS knowingly filled “unlawful prescriptions” for opioids and other controlled substances, and then sought reimbursement for them from federal healthcare programs like Medicaid and Medicare.
CVS and Walgreens are also accused of pressuring their pharmacists into filling prescriptions for opioids and other controlled substances without a thorough review.
In a statement however, Walgreens said many of the federal rules governing pharmacies are so vague as to be impossible to follow.
“We are asking the court to clarify the responsibilities of pharmacies and pharmacists and to protect against the government’s attempt to enforce arbitrary ‘rules’ that do not appear in any law or regulation and never went through any official rulemaking process,” Walgreens said. “We will not stand by and allow the government to put our pharmacists in a no-win situation, trying to comply with ‘rules’ that simply do not exist.
“Walgreens stands behind our pharmacists, dedicated healthcare professionals who live in the communities they serve, filling legitimate prescriptions for FDA-approved medications written by DEA-licensed prescribers in accordance with all applicable laws and regulations.”
Both CVS and Walgreens are accused of filling prescriptions for “dangerous and excessive quantities of opioids,” filling prescriptions too early, and filling prescriptions for opioids, benzodiazepines and muscle relaxants, a three-drug combination known as the “Holy Trinity” that the feds consider dangerous.
The DOJ alleges that, from 2012 through the present, Walgreens knowingly filled millions of prescriptions for controlled substances that lacked a “legitimate medical purpose, were not valid, and/or were not issued in the usual course of professional practice.” The complaint against CVS is nearly identical.
It’s noteworthy that the DOJ claims that both Walgreens and CVS have been filling these prescriptions “through the present,” because when it comes to getting an opioid prescription filled, pain patients find CVS and Walgreens to be the two most difficult pharmacies to work with.
In 2023, PNN conducted a large survey of nearly 3,000 pain patients, and when respondents were asked which pharmacy chain was the most difficult to get an opioid prescription filled, more than half the patients in our survey selected either Walgreens (30%) or CVS (26%).
“Every month when I have to get my medication renewed there is always an issue,” explained one patient. “Walgreens always give people a hard time. I've seen many people standing in line and just walk out.”
“CVS continually gives me a hard time to fill my Rx even though I have been on it for over 7 years. It is either out of stock, or they argue with me about filling it,” another patient told us.
That difficulty is likely tied to the fact that Walgreens and CVS signed the National Opioid Settlement in 2022. As part of the settlement, they agreed to pay more than $10 billion to states, cities and counties that sued them for their alleged roles in causing the opioid epidemic.
The nation’s two biggest pharmacy chains also agreed to watch for suspicious orders, report any “problematic” prescribers, and to strictly limit the amount of opioid pain medication they can dispense in any given month.
Opioids, in effect, are now being rationed to their customers, yet the DOJ is claiming that both pharmacies continue to fill opioid prescriptions too easily.
As a pain patient, I use a small local pharmacy specifically to avoid the issues that are common for patients at large pharmacy chains like Walgreens and CVS. However, that alone doesn’t protect me. When the DOJ goes after large pharmacies, the fear trickles down to the smaller ones as well.
Nearly every month I have some issue getting my prescription filled. They claim they can’t find the prescription in their system, and only “find it” after I go back and forth with them and my doctor on multiple phone calls. Or they claim it’s out of stock, which unfortunately I have no way of checking to see if they’re telling the truth.
Just yesterday I spent all day trying to get my pain medication refilled because the pharmacist claimed she accidentally deleted it from the system. I had to get my doctor to resend it.
Dealing with chronic pain is a struggle in and of itself. The last thing pain patients need is another battle to fight at the pharmacy. If Walgreens and CVS are unsuccessful in fighting back against their respective DOJ lawsuits, it’s likely that pain patients will suffer even more as a result.