Pain Clinic Chain to Pay $11M to Settle Fraud Claims
/By Don Thompson, KFF Health News
The owner of one of California’s largest chains of pain management clinics has agreed to pay nearly $11.4 million to California, Oregon, and the federal government to settle allegations of Medicare and Medicaid fraud.
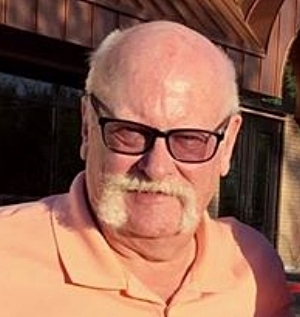
The U.S. Department of Justice and the states’ attorneys general say Francis Lagattuta, a physician, and his Lags Medical Centers performed — and billed for — medically unnecessary tests and procedures on thousands of patients over more than five years.
It was “a brazen scheme to defraud Medicare and Medicaid of millions of dollars by inflicting unnecessary and painful procedures on patients whom they were supposed to be relieving of pain,” Phillip Talbert, U.S. attorney for the Eastern District of California, said in a statement this month.
The federal Medicare program suspended reimbursements to Lags Medical in June 2020, and Medi-Cal, California’s Medicaid program, followed in May 2021. Lags Medical shut down the same day the state suspended reimbursements. The company, based in Lompoc, California, had more than 30 pain clinics, most of them in the Central Valley and the Central Coast.
A KFF Health News review last year found the abrupt closure left more than 20,000 California patients — mostly working-class people on government-funded insurance — struggling to obtain their medical records or continue receiving pain prescriptions, which often included opioids.
Lagattuta and Lags Medical did not admit liability under the settlement. Lagattuta denied the governments’ claims, saying in a statement he was “pleased” to announce the settlement of a “long-standing billing dispute.” As part of the agreement, Lagattuta will be barred for at least five years from receiving Medicare and Medicaid reimbursements.
“Since the Centers have been closed for a couple of years, it made sense for Dr. Lagattuta to settle the dispute and continue to move forward with his other business interests and practice,” Malcolm Segal, an attorney for Lagattuta and the centers, said in the statement.
According to state officials, the federal government will receive the bulk of the money, about $8.5 million. California will receive about $2.7 million, and an additional $130,000 will go to Oregon. The settlement amount is based in part on Lagattuta’s and Lags Medical’s “ability to pay.” It does not cover the governments’ full losses, which the U.S. attorney’s office in Sacramento said are not public record.
Blanket Orders for Unnecessary Tests
A nearly four-year investigation by federal officials and the California Department of Justice found that from March 2016 through August 2021, Lagattuta and his company submitted reimbursement claims for unneeded skin biopsies, spinal cord stimulation procedures, urine drug tests, and other tests and procedures.
Lagattuta began requiring all his clinics to perform various medical procedures on every patient, the officials said, no matter if they were needed or requested by patients’ medical providers. Patients who refused were told they would have their pain medication reduced and could suffer adverse medical consequences.
U.S. and California investigators piggybacked on a federal claim filed in late 2018 by a whistleblower, Steven Capeder, Lags Medical’s former operations and marketing director, who will receive more than $2 million of the settlement.
As part of the settlement, Lagattuta and his company acknowledged that in mid-2016 he began requiring his providers to do at least two to three skin biopsies on Medicare patients each day and told providers to quit if they wouldn’t comply. Such biopsies are used to measure small-fiber neuropathy, which causes burning pain with numbness and tingling in the feet and lower extremities.
According to the settlement, a monthly report in early 2018 set a goal of performing 250 biopsies a week. Lagattuta created a separate team that was required to order at least 150 biopsies weekly, often overruling providers. And the company’s chief executive officer in late 2019 texted Lagattuta to report a particularly high number of biopsies, illustrating the text with emojis of a money bag and a smiley face.
Authorities said Lagattuta violated regulations requiring that skin biopsy results be interpreted by a trained pathologist or neurologist. Instead, they say, Lagattuta had the biopsies read by a family member who had no formal medical training and by a former clinic executive’s spouse, who was trained as a respiratory therapist.
Lags Medical clinics performed more than 22,000 biopsies on Medi-Cal patients from 2016 through 2019.
The settlement also alleges Lagattuta encouraged unsuitable patients to undergo spinal cord stimulation. It describes the procedure as “an invasive surgery of last resort,” in which implants placed near the spinal cord apply low-voltage electrical pulses to nerve fibers.
Lagattuta paid a psychiatrist $3,000 each month to falsely certify that every Lags Medical candidate for the procedure had no psychological or substance use disorders that would negatively affect the outcome, according to the settlement. For instance, the settlement says the psychiatrist overruled a Lags Medical social worker to OK the procedure for a young woman who had bipolar disorder with hallucinations that included hearing a man’s voice ordering her out of bed.
He also issued blanket orders for every patient to have urine drug testing, a policy the company’s CEO said “should be a big money maker.”
KFF Health News found that from 2017 through 2019 nearly 60,000 of the most extensive urine drug tests were billed to Medicare and Medi-Cal under Lagattuta’s provider number. Medicare reimbursed Lagattuta $5.4 million for those tests.
The clinics “carefully examined, tested, and treated” more than 60,000 patients during the time covered by the settlement, “when others might have been content to prescribe medication to mask pain,” said Lagattuta’s statement.
KFF Health News is a national newsroom that produces in-depth journalism about health issues.