All Things Considered: Except Patients
/By Pat Anson, Editor
National Public Radio’s All Things Considered is one of the most respected radio programs in the country, reaching nearly 12 million listeners each week.
So when All Things Considered aired a two-part series this week on the opioid prescribing guidelines being developed by the Centers for Disease Control and Prevention (CDC), many expected an in-depth and balanced report on America’s love-hate relationship with opioids – how a medicine that gives pain relief to millions is also responsible for the deaths of thousands who abuse it.
Host Robert Siegel said the nation was at a “turning point” in its complicated relationship with opioids. The broadcast interviewed pain specialists, a family physician, and various experts who said the CDC guidelines either go too far or are long overdue.
“We have a moral responsibility to address pain and suffering. And we do have a responsibility not to do harm, but you can do harm in either direction,” said Richard Payne, MD, of Duke University.
“The number of deaths is only the tip of the iceberg, that's just indicating the pyramid of problems that lies beneath,” said Jane Ballantyne, MD, President of Physicians for Responsible Opioid Prescribing (PROP).
Completely missing from the report was the voice of pain patients. Many noticed the omission and left comments on NPR’s website.
“Please consider interviewing real chronic pain patients. Everyone seems to be making decisions about our treatment but no one asks us how these medications work for us,” wrote one pain sufferer.
“Sorry but NPR screwed up majorly on this piece – they had no panel of patients to give their thoughts – considering how terrible pain patients are treated, that would have been a good angle,” wrote Cary Brief.
“The recent public discussion on opiates, which paints all opiate users as addicts or drug-seeking, is not only unhelpful, it is exceedingly harmful to patients like myself who take their medications as prescribed,” said a woman who suffers from chronic back pain.
“I am amazed at my beloved NPR not doing their homework on this,” wrote Kristine Anderson. “You have just labeled yourself another media outlet getting your information from only the CDC (other than Dr. Payne perhaps) and creating feed off of their press releases, timely sent just as the guidelines comments were reopened and soon to close.”
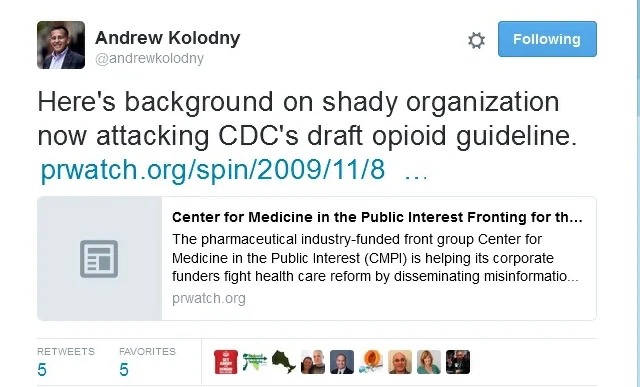
Anderson also wrote she was disappointed that the broadcast included a lengthy interview with Ballantyne, a retired pain specialist who has recently emerged as a controversial figure in the debate over opioids. As Pain News Network has reported, Ballantyne is one of five PROP board members who are advising the CDC and her inclusion in a secret panel of experts is one of the reasons the agency delayed implementing the guidelines and reopened a public comment period.
Critics have said Ballantyne is biased, has a financial conflict of interest, and should be fired from her academic position at the University of Washington School of Medicine for advocating that pain intensity not be treated.
None of that was reported by All Things Considered, which gave Ballantyne a prominent role in the broadcast. Ballantyne told the program that during her lengthy career in pain management she and other doctors were sometimes abused and insulted by “awful” pain patients when they tried to wean them off opiates.
“If you give people opiates, they think you're the best thing since sliced bread. They love you. They just worship the ground you walk on. The moment you suggest that you want to try and get them down on their dose or, worse still, say you can't carry on prescribing - not that I do that myself; I never cut people off; I don't think people should be cut off, but I do try and persuade them to come down on their dose - they are so awful,” Ballantyne said.
“And you can see why people who are not seeped in this stuff - the young primary care physicians just don't know what to make of it. They don't want to be abused. They want to be loved like everybody else does. We go into medicine to try and help people. And when you get abused and, you know, insulted, you can see why it perpetuates itself.”
Ballantyne said patients on high doses of opiates “were absolutely miserable, were not doing well, were medically ill and always had severe pain." It was then that she and her colleagues began to think "the opiate wasn't helping, and maybe it was harming.”
You can listen to Ballantyne in the first part of NPR’s story, by clicking here.
The second part -- an interview with Dr. Wanda Filer, president of the American Academy of Family Physicians -- can be heard by clicking here.