Sales Reps Charged in Fentanyl Kickback Scheme
/By Pat Anson, Editor
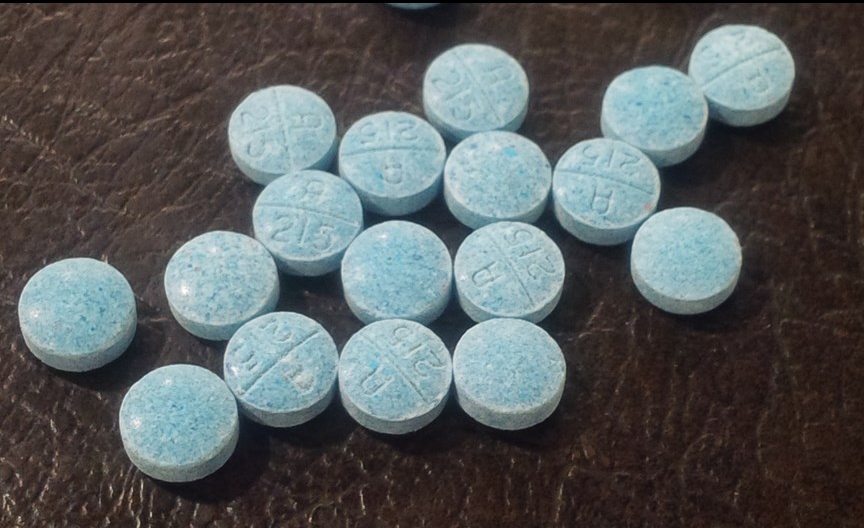
We’ve been reporting recently about illicit fentanyl and how drug dealers were using the potent painkiller to make counterfeit pain medication and selling it on the street, resulting in dozens of overdose deaths.
But drug dealers aren’t the only ones peddling fentanyl illegally and killing people in the process.
Federal prosecutors say two sales reps for Insys Therapeutics broke the law by paying doctors to prescribe Subsys, an oral fentanyl spray sold by the Arizona drug maker. Some doctors were wined and dined at upscale restaurants in New York City, while others were taken to private tables at a strip club, given free booze, and who knows what else.
The sordid details were revealed in a federal indictment handed down last week, which resulted in the arrests of Jonathan Roper and Fernando Serrano.
It’s not the first and probably not the last time Insys has come under scrutiny for unscrupulous marketing tactics or for putting profits ahead of patients. Another former Insys sales representative pleaded guilty to federal kickback charges in February, and the company is under federal and state investigations in Oregon, California, Massachusetts, Connecticut, Arizona and Illinois.
Subsys was approved by the FDA for breakthrough cancer pain, but Insys allegedly pressured its sales representatives to woo or bribe doctors into prescribing Subsys off-label for conditions such as joint pain and post-traumatic stress disorder.
The spray is a lucrative product for Insys and it's biggest moneymaker. According to the Healthcare Bluebook, 30 spray bottles of Subsys cost about $7,300.
“This case should be something the medical industry and the general public should pay close attention to because it’s one of the reasons we’re experiencing an epidemic of overdoses and deaths in this country,” said FBI Assistant Director Diego Rodriguez.
“Not only did the defendants in this case allegedly bully sales reps into pushing this highly addictive drug, they paid doctors to prescribe it to patients. The more prescriptions written, the more money the doctors made. Instead of seeing a way to help people who are dealing with extreme pain, they allegedly saw a huge payday that potentially put people’s lives in danger.”
Since Subsys was introduced in 2012, the FDA’s Adverse Events Reporting System lists over 200 deaths linked to Subsys as the probable cause of an adverse reaction.
According to prosecutors, Roper and Serrano paid two unnamed doctors hundreds of thousands of dollars to make “educational presentations” to other physicians about Subsys. Many of the presentations were nothing more than “social gatherings at high-end restaurants in Manhattan” and some of the physicians were later taken to a strip club, according to prosecutors. Sign in sheets for the presentations were frequently forged to make them appear legitimate
According to the indictment, Serrano was instructed by his sales manager to "expect and demand" that the two doctors hired as speakers prescribe "large quantities" of Subsys. The doctors apparently obliged, prescribing over $5 million worth of Subsys in 2014, much of it billed to private insurers or Medicare.
According to Open Payments, a government website that tracks industry payments to doctors, Insys paid over $7 million to doctors in 2014 for food, beverages, travel, lodging and speaker fees; over ten times what the company reported spending on research. You can see if your doctor took money from Insys and how much by clicking here.
“Jonathan Roper and Fernando Serrano corruptly induced doctors to prescribe millions of dollars’ worth of Fentanyl through thousands of dollars in kickbacks disguised as phony educational programs. As alleged, Roper and Serrano helped feed this devastating surge of opioid addictions by tapping into another age-old addiction, greed,” said U.S. Attorney Preet Bharara.
Roper and Serrano are each charged with one count of conspiracy to violate the federal Anti-Kickback Statute and one count of violating the Anti-Kickback Statute. Each of the two counts carries a maximum term of five years in prison.