1. Check your bag
This is definitely the most important tip I can give you.
Yes, on most airlines it costs a little more, but that’s why God invented Southwest and it’s free checked-bag policy.
And yes, sometimes you get to your hotel only to discover that the mirror in your $32 Urban Decay Naked Flushed compact somehow broke in transit. But there are other mirrors.
And not having to deal with luggage can be the difference between arriving in Phoenix feeling like you’ve just been involved in a plane crash, and arriving in Phoenix feeling like you just got up from a really great nap.
From a practical standpoint, checking your bag means you don’t have to drag it to your terminal or deal with lifting it up into the overhead bin while desperately looking around for help from the other travelers, hoping one of them has the magical ability to see your invisible illness.
And it also means that you’re free to be one of those carefree people boarding the plane holding just a purse and a cell phone. Trust me, it’s the only way to fly.
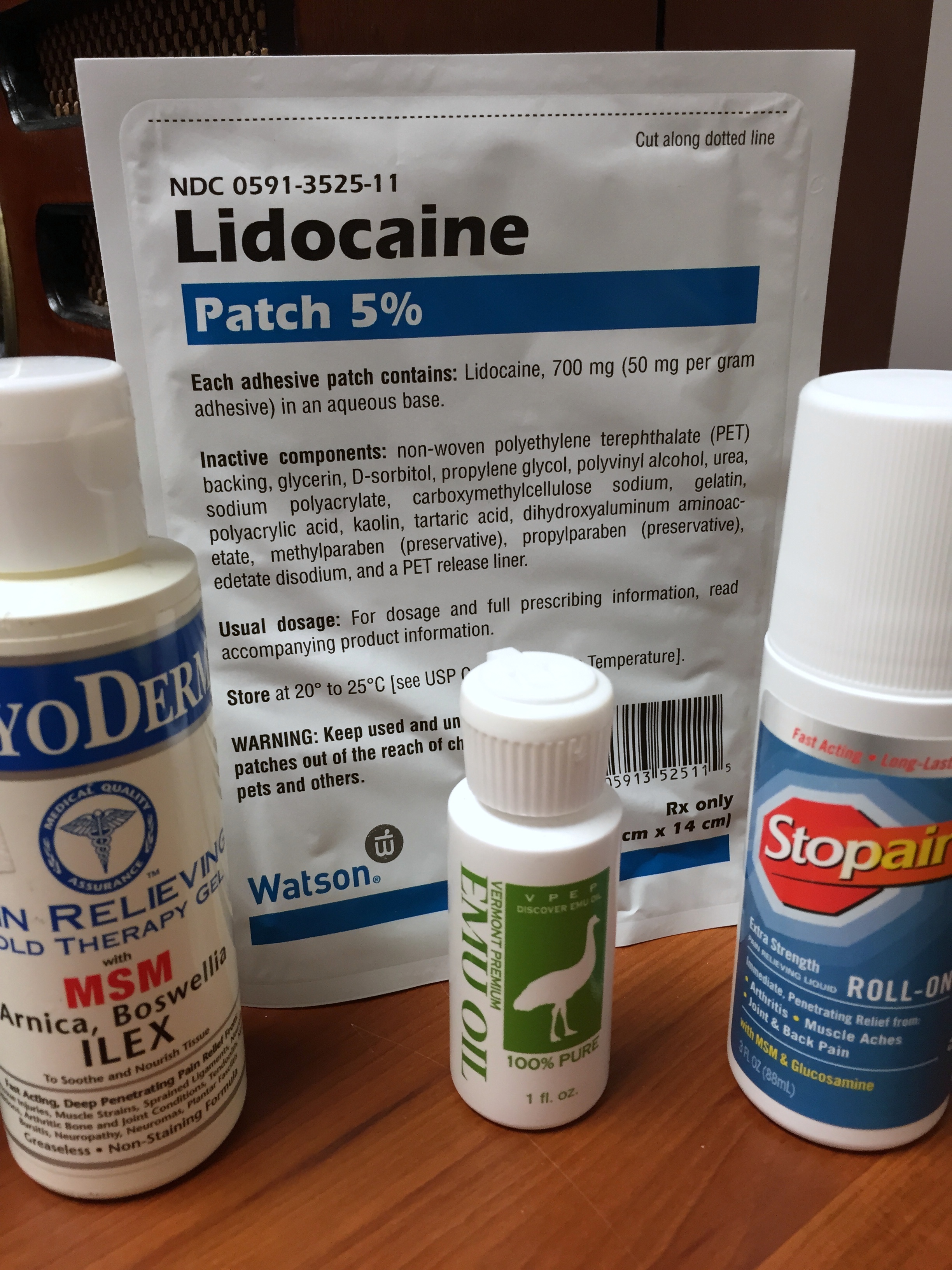
2. Put all your medications in your carry on.
No, seriously, all of them. Even that one you only take right before bed that you don’t think you’ll possibly need before you arrive. And that other one that you definitely don’t think you’ll need because you only take it on Wednesdays and today is Thursday.
While regular people with regular health may think it’s a no brainer to carry-on all your pills, that’s not the case for us. People who deal with chronic pain have a legit chance of needing 23 different prescription bottles daily, so downsizing a carry-on bag by putting a couple of them in the checked luggage doesn’t seem so crazy. Unfortunately, there are so many things that can go wrong.
They could lose your luggage. Or you could miss your connecting flight. Or zombies could attack. So it’s just better to have that hydrocodone in your purse just in case.
And if any of the TSA agents try to give you crap about all that morphine you carry around, just show them your name on the prescription bottle and say, “No, yeah, these are mine. Sorry about that. Thanks for asking though. And also you’re doing a really great job here.”
Because you don’t want to be rude to a TSA agent — those guys have power over the terrorist watch list.
3. Buy the huge Fiji water bottle and drink all of it
The thing is, if you have chronic pain, all those warnings about drinking water to stay hydrated in the sky are even more pertinent.
Sleeping pills, nerve medications and opioids all have the fun side effect of dehydrating you all by themselves, so when you add in recycled air and cabin pressure suddenly you’re so thirsty even a caffeine-free, diet, generic Coke sounds good.
And, here’s what nobody tells you about that — all that dehydration and sitting on a plane in seats too small to bend your ankles makes your feet swell up. It’s a real thing. And it sucks.
So yeah, water, it’s important — especially if you’re planning to wear flip-flops on your trip.
But, as anyone who’s ever had to go through security at the airport will tell you, it’s impossible to get a bottle of any kind of water through the X-ray machine. So if you want to stay hydrated you have to buy something after the checkpoint. And personally, I like to use it as an excuse to splurge on one of those completely impractical square bottles of Fiji.
Hey, if you have to buy a bottle of water, you may as well buy the one that tastes like it came from the Garden of Eden.
4. Pack dry shampoo and skip the showers
When you do finally get to L.A., the Mayo Clinic, or your grandma’s house, the very best thing you can do is skip the shower and just spray a crap ton of dry shampoo on your bangs. Seriously, this has been the BIGGEST lifesaver for me when traveling.
Chronic pain has this way of turning simple showers into some sort of extreme marathon mud run through the Amazon. And while normal people might think they should be fresh and clean when they have a business meeting, people with chronic pain know that it’s more important to actually show up to said business meeting.
Skipping the shower can preserve precious energy that will help you endure the trip, or, you know, maybe even have some fun later on — assuming your sleeping pill hasn’t kicked in yet.
5. Go for the window seat
Even with the pain and the pills and the swollen feet and the missed connections, travel is still travel, and getting to ride on a plane is still pretty cool.
Honestly, window seats aren’t actually practical at all. It’s just that much harder to get up and use the bathroom after downing all that Fiji water, and you have nowhere to run when the old dude sitting next to you starts hitting on you hard core 5,000 feet in the air.
But, window seats are something more important than practical — they’re fun. All you have to do is glance out the window and you’ll get a view most people in human history have never had the chance to experience — whether it’s a blanket of pure white clouds, a bird’s eye look at the people who call this planet home, or just a great play-by-play of the machine you’re riding in gliding toward the heavens.
It’s pretty incredible when you think about it.
And sometimes, every once in a while, something almost magical happens, and you end up in a window seat, in an exit row, AND nobody sits next to you. It’s not quite first class, but it’s close enough.
And when you finally get to wherever you’re going, you can toss that empty bottle of Fiji into the recycling bin, grab your checked-luggage off the carrousel, throw on some sunglasses, and tackle your trip like the chronic pain warrior you are.
Bon Voyage!