A Safe Way to Healthy, Restorative Sleep
/By Ellen Lenox Smith, Columnist
For many of us suffering from chronic pain, coping with our medical issues can be physically and emotionally draining. Often, the lack of healthy sleep is the culprit.
Living with Ehlers Danlos syndrome (EDS) and sarcoidosis, I used to constantly wake up in the middle of the night with so much pain it was impossible to get any form of rest. When I was teaching, I somehow went for years trying to teach on “empty” due to a chronic lack of restorative sleep.
I remember having to cheat and use a seating chart to remember the names of my wonderful students, who were sitting right in front of me. These were students I had known, loved and taught for months. It was embarrassing, heartbreaking, and created a sense of loss and hopelessness.
Thankfully, those days are gone. I have gone from years of almost no quality sleep to being someone who goes to bed at night and wakes up in the morning feeling well rested. I don’t even remember any dreams, so I am getting the real REM sleep!
How did I do it? A teaspoon of oil made from medical marijuana. I take it before bedtime, mixed with a little applesauce or a small amount of food.
Within an hour, my body is ready for bed and sleep.
For years I made this oil at home on top of the stove, but today enjoy using the Magical Butter machine. We find that oil made from the indica strain of marijuana works best for sleep. Directions for making the oil can be found on our website.
I am now both a medical marijuana patient and a caregiver in the state of Rhode Island. Patients visit us with a variety of different illnesses, but the one thing they all have in common is lack of sleep. Without sleep, you lose hope and courage to move forward with your life. Each patient that has tried this oil has found that it gives them rest and hope.
Recently, a young woman and her husband came to our home. Living with both EDS and Chronic Regional Pain Syndrome (CRPS), she had a difficult life, but was hoping to find something to make it easier. We have the same pain doctor and he suggested she get in touch with us to learn about cannabis.
The first night that she tried the oil, she slept for eight hours and was both thrilled and shocked. She said even her face looked calmer and more rested. She is now happier, hopeful and has more strength to get through the day.
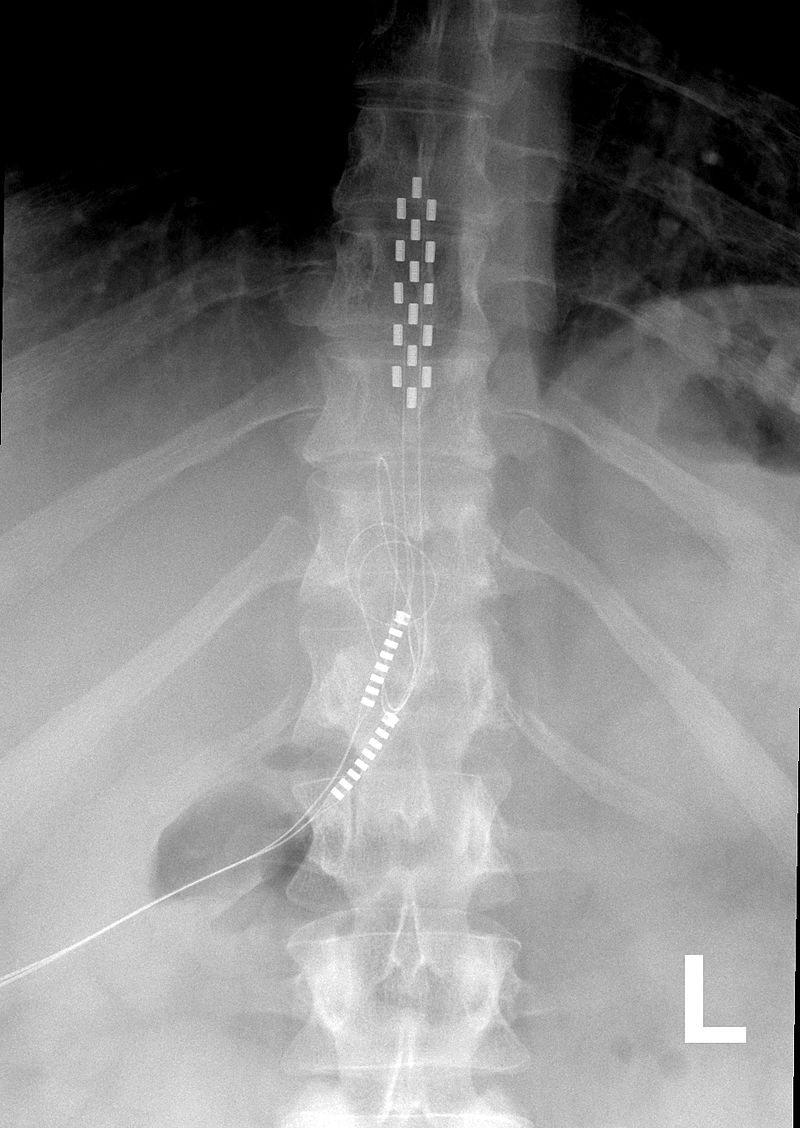
There was another patient sent to us who was a paraplegic in constant pain. He was angry, miserable and wished he hadn’t been given life-saving surgery after his accident. He was at a loss as to what to do to cope with the life he was now given.
He tried the oil and was shocked what it did for him. From that point on, the desperate man who first called me and couldn’t even be understood due to his level of pain, was happy, laughing and finding some meaning in his difficult life. He later passed, but the oil gave him a better quality of life and a sense of purpose again.
We have seen one success after another of pain patients getting real quality sleep and rest. We have seen it work for cancer patients, and those suffering with post-traumatic stress disorder, multiple sclerosis, back pain, fibromyalgia, arthritis and other conditions.
For those of you who are caught up in opioid hysteria and can no longer get medication, I hope you take a moment and think about trying cannabis oil at night for rest. I have used it safely for a decade, since I am not able to metabolize even an aspirin or Tylenol, let alone any opiate. May you find the courage to try it and get the same results.
Ellen Lenox Smith suffers from Ehlers Danlos syndrome and sarcoidosis. Ellen and her husband Stuart are co-directors for medical marijuana advocacy for the U.S. Pain Foundation and serve as board members for the Rhode Island Patient Advocacy Coalition.
For more information about medical marijuana or to contact the Smith's, visit their website.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.