What is Opioid Use Disorder?
/By Rochelle Odell, Columnist
You’ve probably heard or seen the phrase “Opioid Use Disorder.” It’s a broad term currently being used to describe not only opioid addiction, but patterns of behavior that might be a sign of addiction or could lead to it.
If that sounds like they’re putting the cart before the horse, it’s because they are.
In order to understand Opioid Use Disorder, one must understand the government's stance on opioids. The National Institute on Drug Abuse – which is part of the National Institutes of Health (NIH) – lays it out in a recently revised statement on the opioid crisis:
“Every day, more than 90 Americans die after overdosing on opioids. The misuse of and addiction to opioids--including prescription pain relievers, heroin and synthetic opioids such as fentanyl--is a serious national crisis that affects public health as well as social and economic welfare."
Notice how they lump prescription pain relievers in with heroin and illicit fentanyl? The more I research, the more I find this common thread of illogical thinking. The government consistently lumps pain medication in with illicit drugs.
Here’s another example from the NIH:
“In 2015, more than 33,000 Americans died as a result of an opioid overdose, including prescription opioids, heroin, and illicitly manufactured fentanyl, a powerful synthetic opioid.
That same year, an estimated 2 million people in the United States suffered from substance use disorders related to prescription opioid pain relievers, and 591,000 suffered from a heroin use disorder.”
Substance use disorders “related” to pain relievers? Heroin use disorder? That got me wondering how many drug “disorders” there are.
According to the Substance Abuse and Mental Health Services Administration (SAMSHA), there are six major substance use disorders. Nearly 93,000,000 Americans have a substance use disorder of some kind:
1) Alcohol Use Disorder (AUD): About 17 million Americans have AUD. According to the CDC, alcohol causes 88,000 deaths a year.
2) Tobacco Use Disorder: Nearly 67 million Americans use tobacco. According to the CDC, cigarette smoking causes more than 480,000 deaths a year.
3) Cannabis Use Disorder: Over 4 million Americans meet the criteria for a substance use disorder based on their marijuana use. No estimate is provided on the number of deaths caused by marijuana, if any.
4) Stimulant Use Disorder: This covers a wide range of stimulant drugs that are sometimes used to treat obesity, attention deficit hyperactivity and depression. The most commonly abused stimulants are amphetamine, methamphetamine and cocaine. Nearly 2 million Americans have a stimulant use disorder of some kind.
5) Hallucinogen Use Disorder: This covers drugs such as LSD, peyote and other hallucinogens. About 246,000 Americans have a hallucinogen use disorder.
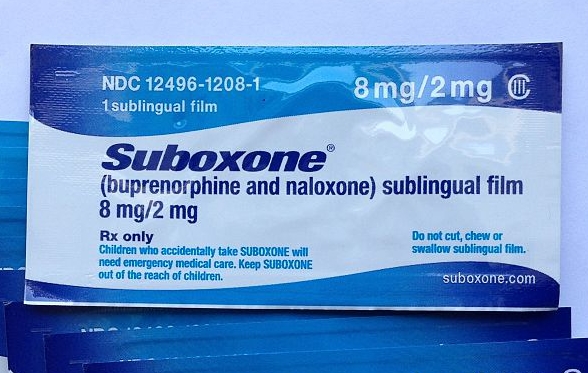
6) Opioid Use Disorder: Again, this covers both illicit opioids and prescription opioids. In 2014, an estimated 1.9 million Americans had an opioid use disorder related to prescription pain relievers and 586,000 had a heroin use disorder (notice the SAMSHA numbers are somewhat different from what the NIH tells us).
But what exactly is Opioid Use Disorder? Does it mean 2.5 million Americans are addicted to opioids?
No.
The diagnostic codes used to classify mental health disorders were revised in 2013 to cover a whole range of psychiatric symptoms and treatments. Two disorders – “Opioid Dependence” and “Opioid Abuse” -- were combined into one to give us “Opioid Use Disorder.” Few recognized at the time the significance of that change, it's impact on pain patients, or how it would be used to inflate the number of Americans needing addiction treatment.
Elizabeth Hartley, PhD, does a good job explaining what Opioid Use Disorder is in an article for verywell.
Hartley wrote that Opioid Use Disorder can be applied to anyone who uses opioid drugs (legal or illegal) and has at least two of the following symptoms in a 12 month period:
- Taking more opioids than intended
- Wanting or trying to control opioid use without success
- Spending a lot of time obtaining, taking or recovering from the effects of opioids
- Craving opioids
- Failing to carry out important roles at home, work or school because of opioid use
- Continuing to use opioids despite relationship or social problems
- Giving up or reducing other activities because of opioid use
- Using opioids even when it is unsafe
- Knowing that opioids are causing a physical or psychological problem, but using them anyway
- Tolerance for opioids.
- Withdrawal symptoms when opioids are not taken.
The last two criteria will apply to almost every chronic pain patient on a prescription opioid regimen. So might some of the others. Most of us develop a tolerance for opioids, and if they are stopped or greatly reduced, we will experience withdrawal symptoms. We simply cannot win for losing.
If you learn your physician has diagnosed you with Opioid Use Disorder, be sure to ask them what criteria were used and why was it selected. Ask if you should see a doctor more knowledgeable about diagnostic codes and psychiatric disorders.
Remember, knowledge is power. Take this information with you on your next visit to the doctor if you suspect you have been diagnosed with Opioid Use Disorder and your medications have been cut or reduced.
I hope what I have written helps you further understand exactly what we are facing and why. To be honest, it makes me want to wave the white flag, but I know that cannot happen. We have to fight. Fight for proper care for a chronic disease or condition we didn't ask for or want. We can’t live the rest of our lives in severe, debilitating pain when effective treatment is available.
Rochelle Odell lives in California. She’s lived for nearly 25 years with Complex Regional Pain Syndrome (CRPS/RSD).
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.