There’s Still Plenty of Stigma About Opioid Addiction
/By Crystal Lindell
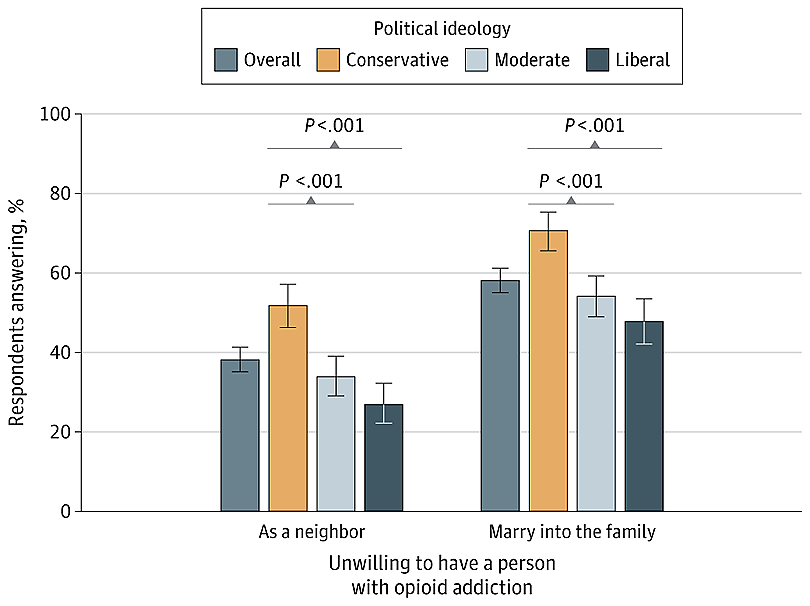
Many Americans still view opioid addiction as a stigmatized condition – with over half (58%) saying they wouldn’t want someone with an opioid use disorder marrying into their family. And over a third (38%) don’t want to be neighbors with someone with opioid addiction.
That’s according to an online survey of over 1,550 U.S. adults by researchers at Cornell University, who published their findings in JAMA.
The goal of the survey was to see how Americans view opioid overdose deaths, people with opioid addiction, and who is responsible for solving the opioid crisis. They also measured if views differed by political ideology.
Notably, the survey did not define “addiction” before asking questions about it, leaving it up to each respondent to rely on their own personal perception of what addiction is. There are issues with that approach, as many people don’t know the difference between addiction and dependence, which is a reliance on medication to treat a health condition.
The survey also didn’t distinguish between people addicted to prescription opioids and those addicted to illicit opioids such as fentanyl or heroin. Most U.S. overdoses involve illicit fentanyl.
That said, the responses indicate that many people view opioid addiction through an ideological lens.
There was broad agreement among conservatives, moderates and liberals that opioid overdose deaths are a serious problem. Overall, 88% rated it as a very serious problem.
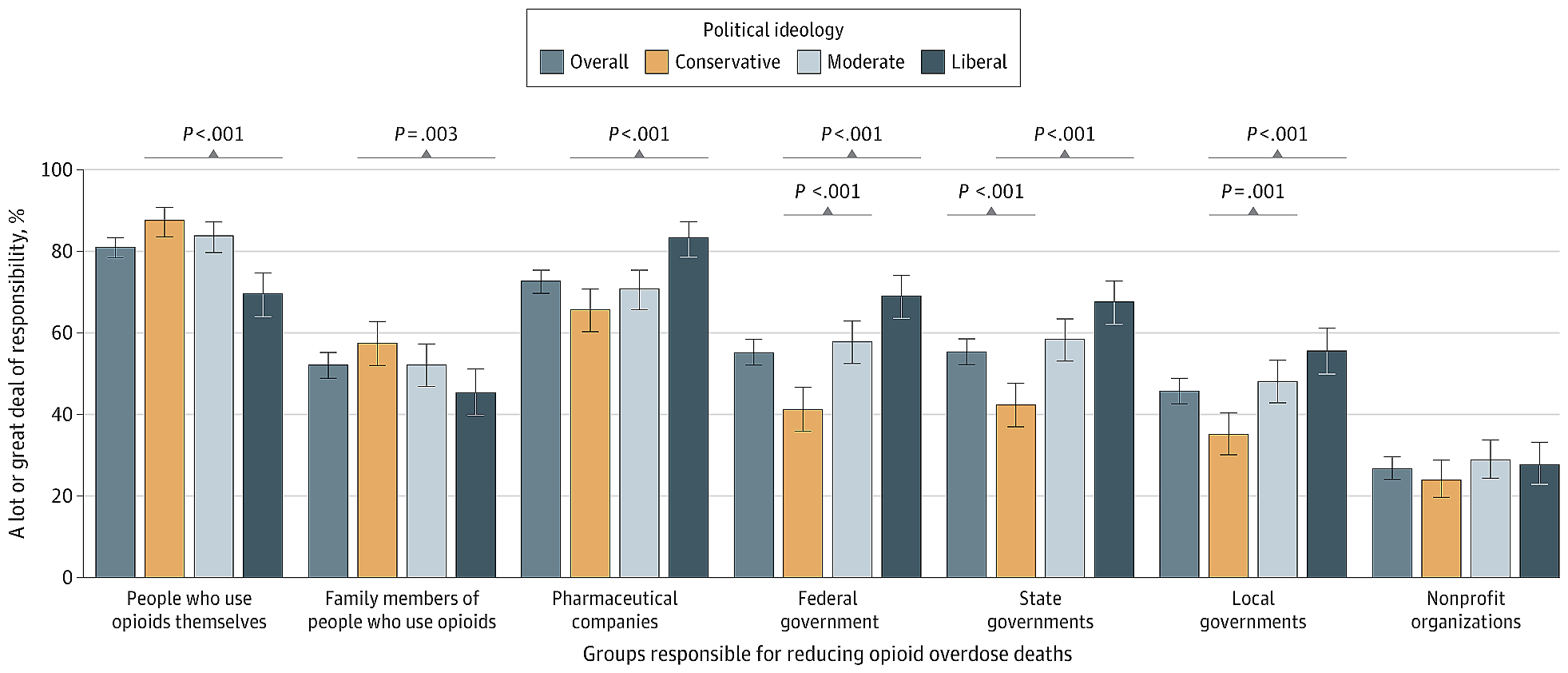
But when it comes to responsibility for reducing overdose deaths, conservatives were more likely than liberals to say people who use opioids and their family members bear a personal responsibility for reducing the number of deaths.
Liberals, on the other hand, were more likely than conservatives to say pharmaceutical companies, as well as federal, state and local governments, were responsible for fixing the problem.
Only about one in four thought that nonprofit organizations were responsible for the opioid crisis.
Perceived Responsibility for Reducing Opioid Overdose Deaths
SOURCE: jama
Conservatives were also more likely to have a stigmatized view of people with opioid use disorder. Over half of conservatives (52%) said they were unwilling to have a neighbor with an opioid addiction (compared to 27% of liberals), and 71% of conservatives said they would not want someone with an opioid addiction to marry into their family (compared to 48% of liberals).
Attitudes About People With Opioid Addiction
SOURCE: jama
The findings highlight just how widespread the stigma still is when it comes to opioid use.
"It remains striking that nearly one-half of self-described liberals indicated unwillingness to have a person with opioid addiction marry into their family," wrote Harold Pollack, PhD, a Professor of Public Health at the University of Chicago, in a commentary also published in JAMA. "The stigma of current opioid addiction crosses political lines."
Respondents who have a personal experience with opioids — who experienced opioid addiction themselves, had a family member or close friend with addiction, or knew someone who died from overdose — showed a greater willingness to have a person with opioid addiction as a neighbor or in-law.
Interestingly, people with that lived experience were slightly more likely than others (82.2% vs 79.3%) to state that people who use opioids are responsible for reducing opioid overdose deaths.
In his commentary, Pollack said the findings carry important implications for public health messaging regarding harm reduction programs such as free syringes, naloxone distribution, and fentanyl test strips.
"These evidence-informed interventions face continued resistance, most notably from communities and families that experience direct harms arising from the opioid epidemic, who are understandably drawn to abstinence-based approaches rather than to approaches that some perceive as encouraging continued drug use or as replacing one addiction with another," Pollack said.
The survey findings are a subset of data drawn from a much larger survey designed to test public messaging campaigns about Medicaid programs that treat substance use disorder.