Purdue Settles OxyContin Lawsuit for $24 Million
/By Pat Anson, Editor
Purdue Pharma has agreed to pay the state of Kentucky $24 million for misleading consumers about the risks of addiction to OxyContin. The settlement is the latest chapter in Purdue’s seemingly endless string of lawsuits over its popular and potent painkiller.
“Purdue Pharma created havoc in Kentucky, and I am glad it will be held accountable,” said Kentucky Attorney General Jack Conway. “Purdue lit a fire of addiction with OxyContin that spread across this state, and Kentucky is still reeling from its effects.”
Purdue did not admit to any wrongdoing in the settlement.
OxyContin was introduced in 1996 and soon became a blockbuster drug for Purdue, reportedly generating profits in excess of $10 billion. Many critics believe the drug also helped trigger an “epidemic” of opioid addiction and overdoses, causing the deaths of thousands of people nationwide.
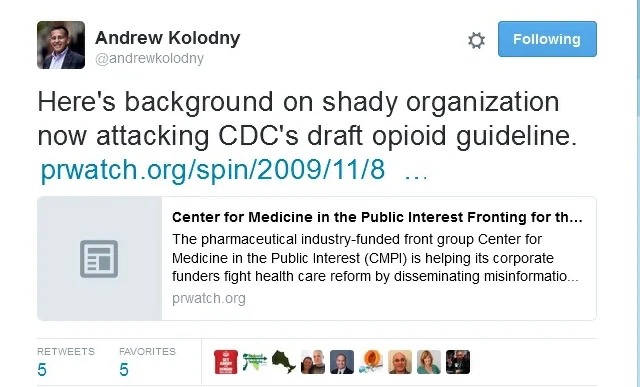
Kentucky filed suit against Purdue in 2007 after company executives pleaded guilty in Virginia federal court to a felony count of falsely marketing OxyContin. Company sales representatives were encouraged to tell doctors the pain medication wasn’t additive and was less likely to be abused.
Purdue settled that case for $634 million and offered $500,000 to Kentucky, which the state refused.
This week’s $24 million settlement is over 50 times what Kentucky was originally offered. The money will be used to fund addiction treatment programs in Kentucky.
Purdue is still fighting a similar OxyContin lawsuit in Chicago. Another case in California was dismissed over the summer.
The original version of OxyContin could be easily crushed and liquefied by addicts to inject or snort for a quick high. OxyContin is now sold in an abuse deterrent formula that is harder to abuse.
“We are pleased to resolve this matter that arose from alleged conduct dating before July 2001, and long before we reformulated OxyContin to include abuse-deterrent properties. This enables Purdue to focus on bringing additional innovative abuse-deterrent medicines to patients,” stated Philip C. Strassburger, Purdue Pharma’s General Counsel.
The reformulation hasn’t stopped the abuse of OxyContin. According to a large nationwide survey of nearly 11,000 opioid addicts who entered a treatment facility in 2012, over a quarter had used OxyContin at least once to get high in the previous 30 days.
Nearly 1,100 people died of overdoses in Kentucky last year, giving the state the dubious distinction of having the 4th highest overdose rate in the country. Many of those deaths are blamed on heroin, as well as prescription opioids.
Purdue as recently as this year was still trying to rein in aggressive marketing by its sales staff. In August, Purdue reached a settlement with New York’s Attorney General, admitting that its sales representatives contacted doctors in New York who were on a “No Call List.” The doctors had been red flagged by the company for possible abuse and diversion of opioids.
Purdue’s sales representatives, who amazingly were not required to check the company's No Call List, made over 1,800 sales calls to doctors on the list, even buying meals for about a third of them. Some of those doctors were later arrested or convicted for illegal prescribing of opioids.
A company spokesman told Pain News Network that sales calls could have also been made to doctors on Purdue No Call Lists outside of New York.
Under the terms of the settlement, Purdue agreed to adopt more “red flags” to identify doctors who may be prescribing opioids inappropriately or illegally. Sales representatives will also be required to check the No Call List before contacting a provider and will be disciplined if they don’t