Canada Fights Wave of Fake Pain Pills
/By Pat Anson, Editor
Canada’s Healthy Ministry today added a dangerous synthetic opioid – known as W-18 -- to a list of illegal controlled substances after the drug was found in counterfeit pain medication sold on the street.
W-18 has been used recreationally in Europe and Canada over the past two years. Recently, Canadian law enforcement have found W-18 disguised to look like legitimate prescription pain medication, such as oxycodone. W-18 is believed to be manufactured in China. It is blamed for one overdose death in Calgary.
"Substances like W-18 are dangerous and have a significant negative impact on some of the most vulnerable people in our society,” said Jane Philpott, Canada’s Minister of Health.
Classifying W-18 as a Schedule I controlled substance – the same class as heroin and cocaine -- makes its production, possession, importation and trafficking illegal in Canada. W-18 was originally developed in the 1980’s as a pain reliever at the University of Alberta, but was never marketed commercially. It is 100 times stronger than fentanyl, another synthetic opioid that is also increasingly being disguised as pain medication and sold on the street.
A Health Canada analysis of counterfeit oxycodone and Percocet pills confirmed the presence of W-18 last month, according to The Globe and Mail.
“Of particular concern is a green coloured oxycodone tablet marked CDN80,” said Corporal Eric Boechler of the Royal Canadian Mounted Police. "It was discontinued as a prescription tablet in 2012, so virtually any encountered on the street today are counterfeit and will contain fentanyl and/or other potent synthetic opioids such as W-18.”
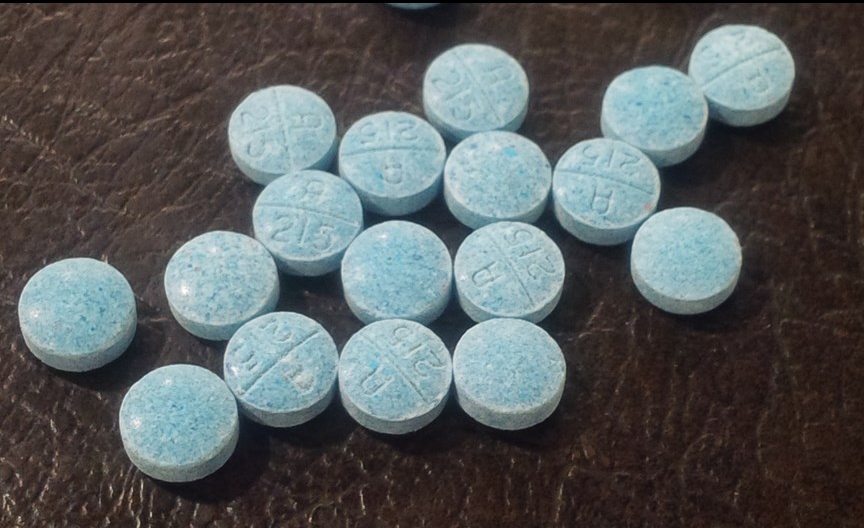
Last week police in North Bay, Ontario seized hundreds of fake fentanyl pills that were disguised to look like 30 mg oxycodone prescription pills. The pills are blue and imprinted with “A 215.”
Counterfeit fentanyl pills have previously been found in western Canada, where they are blamed for dozens of overdose deaths. This was the first time they were found in North Bay, according to BayToday.
“I don’t think these illicit pills coming in from China are aimed at pain patients," said Barry Ulmer, Executive Director of the Chronic Pain Association of Canada.
NORTH BAY POLICE PHOTO
"They appear to be aimed at those who are willing to try ‘new’ things and the usual addiction population. I don’t know what possesses the younger groups to try this stuff from the street as they know full well what could happen.”
As Pain News Network has reported, fake fentanyl pills have also been appearing in the United States, where they are blamed for at least 14 deaths in California and 9 in Florida. Some pills were purchased off the street by pain patients who were unable to get prescription medication through a doctor.
Massachusetts and Rhode Island have both reported an “alarming” rise in fentanyl overdoses. Over half the opioid overdose deaths in those states are now blamed on illicit fentanyl, not prescription pain medication.