Why Aren’t Pain Patients Protesting?
/By Mary Maston, Guest Columnist
I’ve become somewhat disenchanted with my role as a pain patient advocate. When I started out in 2011, I was armed with a strong opinion, an admittedly big mouth, and I suppose I had grand illusions of working with others to effect positive change.
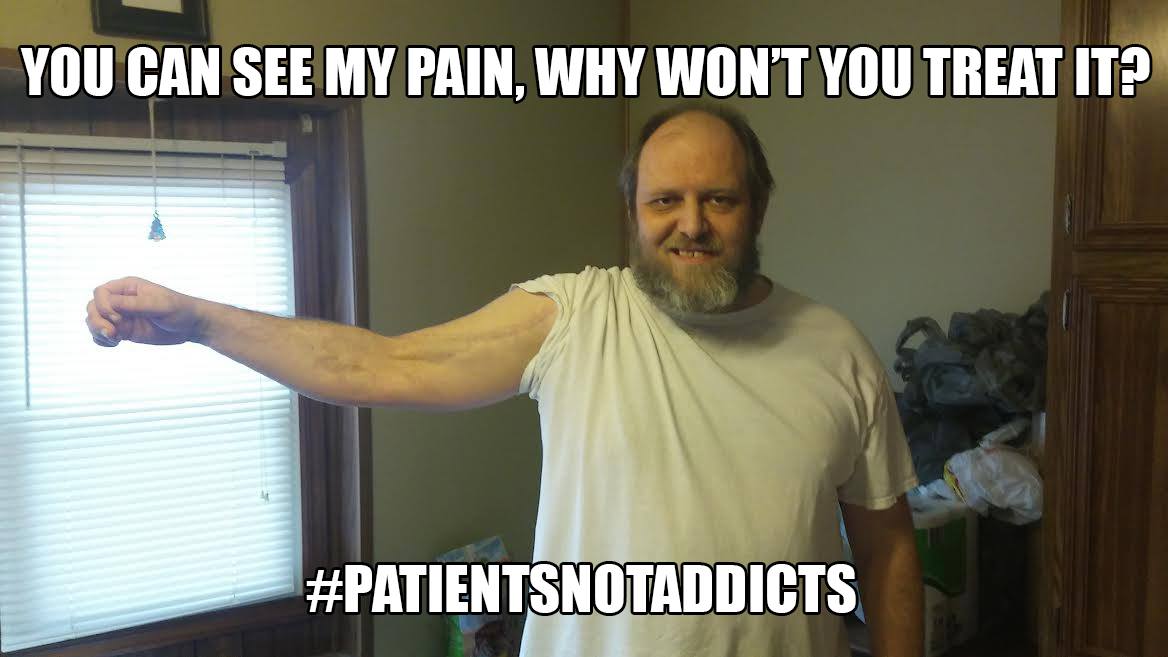
I wanted to help right the wrongs being inflicted on people who depend on pain medication -- not because they want to -- but because of some catastrophic life event that forced them to choose between taking medication to be able to function in their lives or not being able to function at all.
I’ve been there myself. I’m still there and always will be because my kidney diseases are never going away.
Throughout this journey, I’ve had the opportunity to converse with and learn from some highly educated and well versed people in the pain community. Watching them do what they do to help others is nothing short of awe inspiring, and it has helped to keep me going. For that, I can never thank them enough.
The one thing that’s been drilled into my head all these years and has been mentioned in just about every article I’ve ever read about chronic pain is the number 100,000,000.
ONE HUNDRED MILLION. That’s supposedly how many chronic pain patients there are in the United States. If you believe that statistic, we make up nearly a third of the population of the entire country.
So my question is this: WHERE THE HELL ARE YOU??
I read most of the articles that are published on pain and/or pain meds, and all of the comments on both the articles and on Facebook, if that’s where the article is posted. For the most part, I see the same names commenting over and over. Kudos to those who stay persistent, but where are the rest of you?
ONE HUNDRED MILLION and the author is really lucky if he/she gets a couple hundred comments. Usually 30-40 is the going rate. Sometimes it’s even less than that. You can’t blame those who don’t have an internet connection either. Just about everyone has a phone or tablet these days and even elderly people are online in record numbers.
Maybe it wouldn’t have made much of a difference, but maybe it would have if the CDC opioid guidelines had gotten more of a response than they did. We’ll never know now. Where were you when the CDC was taking public comments? I can’t remember the final number, but I know for sure that they received less than 5,000 comments, and many of those comments were people who were in favor of the guidelines – people working against you and the advocates that are trying to go to bat for you.
I personally shared the CDC comment link repeatedly in my Facebook group and practically begged people to write a comment and share their experiences. From talking with other administrators of other groups in the past, I’m sure they all did too. Only a small handful from my group wrote a comment, and by small handful, I mean less than 20.
To say I was disappointed with the final number of comments from patients is an understatement, but what’s done is done and now we all have to live with the outcome.
ONE HUNDRED MILLION - WHERE ARE YOU?
There’s another petition to the White House that’s been active since May 3, asking all of the government entities, including the President, to take pain patients and what we are going through into account by revising the CDC guidelines. It’s been online for 14 days now and only has about 600 signatures. It needs 100,000 to reach the White House.
ONE HUNDRED MILLION - WHERE ARE YOU?
The bottom line is this: We as advocates are doing the best we can and are trying to help you, but we can’t do it by ourselves. Make no mistake, we are rapidly losing this battle and in the end, you are the ones that are going to lose big. Venting in closed Facebook groups is great if it makes you feel better, but complaining in a closed group about not getting your meds to people who can do nothing about it does absolutely NOTHING to contribute to solving the problem. Neither does posting comments on Facebook. You have to go beyond that.
When we use that number, 100 MILLION, and then something big comes along like the CDC guidelines or petitions to the White House and you all don’t step up, it makes us look like we’re just pulling that number out of our rear ends -- like we’re lying.
What are we fighting for if we can’t produce the numbers to back it up? Just my opinion, but if you feel you’ve been wronged because you can’t get the meds you need, I shouldn’t have to beg you to help me fight for you.
I may be mistaken, but I get the impression more and more that other advocates are starting to feel this way as well. How can you help people that aren’t willing to do anything to help themselves? The answer is simple. You can’t.
We know you’re out there and we know what you’re going through; you write to us and tell us. Why won’t you take it further? We only have so many tools we can use, and it’s only going to get worse if you aren’t willing to lend your voices and your signatures to the things we are trying to use to fight for you.
ONE HUNDRED MILLION – that’s a huge number. Imagine what we could do if we all stood united and took a stance. That number of voices is hard to ignore. SO WHERE ARE YOU?
Mary Maston suffers from a rare congenital kidney disease called Medullary Sponge Kidney (MSK), along with Renal Tubular Acidosis (RTA) and chronic cystitis. Mary is an advocate for MSK and other chronic pain patients, and helps administer a Facebook support group for MSK patients.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.