Senators Propose Tax on Opioid Pain Meds
/By Pat Anson, Editor
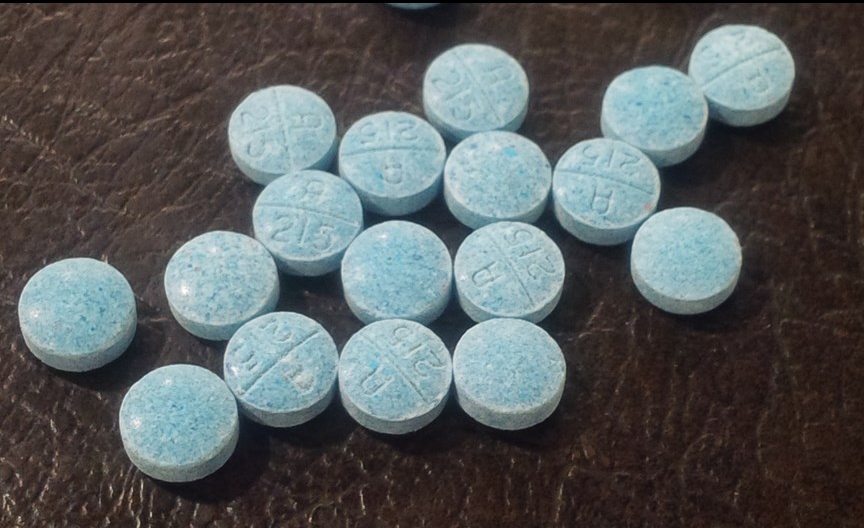
A group of U.S. Senators has introduced legislation that would establish a federal tax on all opioid pain medication. If approved, it would be the first federal tax on a prescription drug levied directly on consumers.
The bill, called the Budgeting for Opioid Addiction Treatment Act, would create a one cent fee on each milligram of an active opioid ingredient in pain medication. Money from this “permanent funding stream” would be used to provide and expand access to addiction treatment.
“A major barrier that those suffering from opioid addiction face is insufficient access to substance abuse treatment,” said Sen. Joe Manchin (D) of West Virginia. “This legislation will bridge that gap and make sure that we can provide treatment to everyone who makes the decision to get help. I look forward to working with my colleagues to get this bill passed so we can take another step forward in the fight against opioid abuse.”
Sens. Amy Klobuchar (D-MN), Jeanne Shaheen (D-NH), Angus King (I-ME), Heidi Heitkamp (D-ND), Tammy Baldwin (D-WI) and Bill Nelson (D-FL) are co-sponsoring the bill, which has been dubbed the “LifeBOAT” Act.
“By establishing a reliable stream of funding, this bill will bolster treatment facilities across the country, increase the amount of services available, and support people as they fight back against addiction – all while doing so in a cost-effective way,” said Sen. King.
The opioid tax would raise an estimated $1.5 billion to $2 billion per year. In an interview with the Portland Press Herald, King said the fee would range between 75 cents and $3 for a 30-day prescription, depending on the dose. He claimed many patients wouldn’t have to pay the additional cost because their insurance would cover it.
King said treatment programs need funding, and tacking the cost onto the price of the drug is a fair way to do it, much like automakers are required to install seat belts and air bags in vehicles.
“The obvious way to fund this is to build it into the price of the drug,” said King. “The cost of the drug should reflect the danger of the drug.”
Although most of the press releases and public statements from the senators avoid using the word “tax” and refer to it as a fee, the bill itself doesn’t hide behind semantics. The legislation would apply to the sale of “any taxable active opioid” and would amend the Internal Revenue (IRS) Code to make it possible.
The federal government and the vast majority of states do not levy a sales tax on prescription drugs. Only two states, Illinois and Georgia, currently have a sales tax on prescription medication.
"I don't understand how, in a world where we are getting upset about the 'tampon tax' we find it perfectly socially acceptable to tax chronic pain patients to pay for addiction treatment," said Amanda Siebe, who suffers from Chronic Regional Pain Syndrome (CRPS) and is a founder of the advocacy group #PatientsNotAddicts.
"With less than 5% of chronic pain patients becoming addicted to opiates, this leave the other 95%, who are often some of the poorest in America and have nothing to do with addiction or addiction treatment, to pick up the tab for addiction treatment. I find myself truly disappointed and ashamed of our government. This tax is discriminatory and we are going to fight it."
The LifeBOAT Act would exempt buprenorphine, an opioid used to treat addiction, from taxation, as well as all over-the-counter pain relievers such as acetaminophen. Cancer and hospice patients would be exempted from the opioid tax, although they would have to apply for a rebate to get their money back.
“The discount or rebate mechanism shall be determined by the Secretary of Health and Human Services with input from relevant stakeholders, including patient advocacy groups. The discount or rebate shall be designed to ensure that the patient or family does not face an economic burden from the tax,” a fact sheet on the bill states.
Sen. Manchin told to his colleagues that there would be little or no opposition to the bill.
“There’s not one person who will lose a vote over this. Not one person. You won’t be accused of voting for a tax,” Sen. Manchin said during a news conference announcing the bill. He noted that no Republican senators have signed on as co-sponsors.
“This is something that’s much needed, overdue and they all recognize it, but they’re scared to death. They’ve taken the (no tax) pledge. They’re scared to death somebody will use it against them. I’ll be standing beside my Republican colleagues if any Democrat tried to attack them and said they tried to vote for a tax,” Manchin said.
To read the full text of the bill, click here.
To watch a video of the press conference, click here.