Virtual Reality Relieves Pain in Hospitalized Patients
/By Pat Anson, Editor
Virtual reality therapy significantly reduced both acute and chronic pain in hospitalized patients, according to a new study that adds to a growing body of evidence that virtual reality (VR) can give temporary relief to pain patients. The study is published online in the journal JMIR Mental Health.
Researchers at Cedars-Sinai Medical Center in Los Angeles enrolled 100 patients in the study who had an average pain score of 5.4 on a pain scale of zero to 10.
They suffered from a wide variety of conditions, including gastrointestinal, cardiac, neurological and post-surgical pain.
Fifty patients watched a 15-minute nature video on a computer screen that included mountain scenes and running streams, accompanied by calming music.
The other 50 patients wore virtual reality goggles to watch a 15-minute animated game called Pain RelieVR, which was specifically designed to treat patients who are bed bound or have limited mobility.
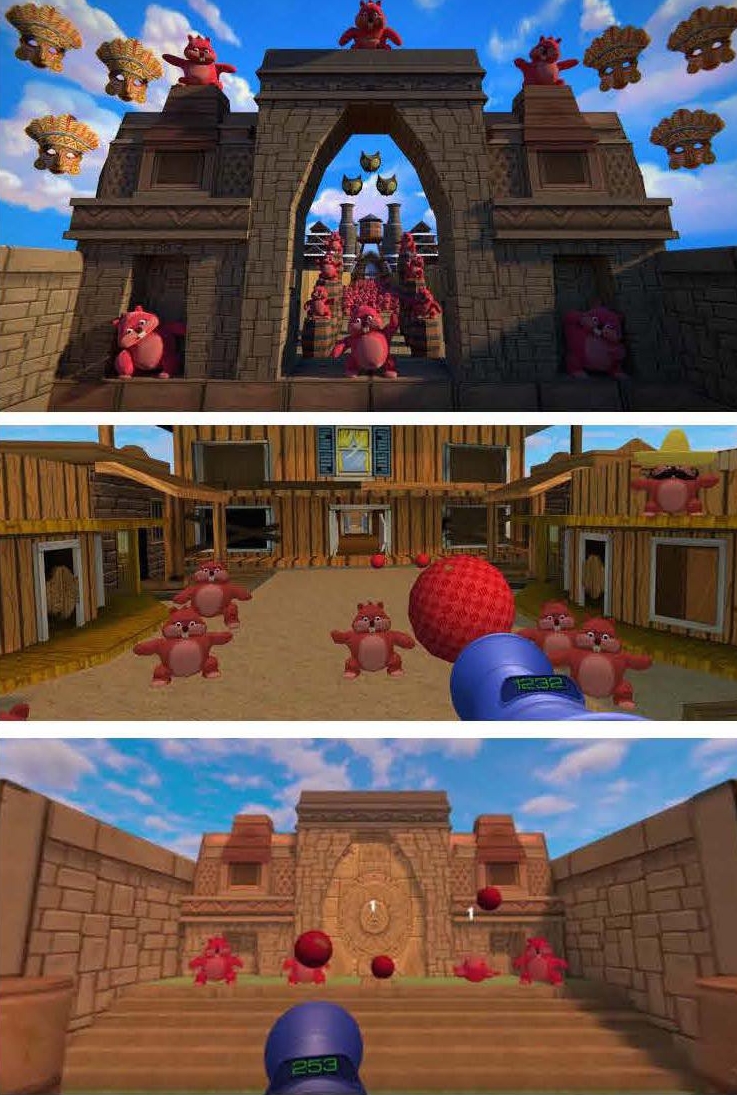
The game takes place in a fantasy world where users shoot imaginary balls at a wide range of moving objects by maneuvering their heads toward the targets. The game also uses motivational music, positively reinforcing sounds and direct messages to patients.
The patients who watched the nature video had a 13 percent drop in their pain scores, while patients who watched the virtual reality game had a 24 percent decline in their pain levels. The VR group had no change in their blood pressure or heart rate.
“We found that use of a 15-minute VR intervention in a diverse group of hospitalized patients resulted in statistically significant and clinically relevant improvements in pain versus a control distraction video without triggering adverse events or altering vital signs,” wrote lead author Brennan Spiegel, MD, director of Cedars-Sinai’s Health Service Research.
“These results indicate that VR may be an effective adjunctive therapy to complement traditional pain management protocols in hospitalized patients.”
scenes from virtual reality game
Researchers say it’s unknown exactly how VR works to reduce pain levels, but one explanation is simple distraction.
“When the mind is deeply engaged in an immersive experience, it becomes difficult, if not impossible, to perceive stimuli outside of the field of attention. By ‘hijacking’ the auditory, visual, and proprioception senses, VR is thought to create an immersive distraction that restricts the mind from processing pain,” said Spiegel.
Because the VR therapy was only 15 minutes long, Spiegel says lengthening the period of pain reduction might require sustained and repeated exposure to a variety of virtual reality content.
Another small study of VR therapy, published in PLOS, found that just five minutes of exposure to a virtual reality application reduced chronic pain by an average of 33 percent.
VR therapy is not for everyone. It may induce dizziness, vomiting, nausea or epileptic seizures, so patients have to be screened and monitored for side effects. Another barrier is age related. Two-thirds of the people who were eligible for the Cedars-Sinai study were unwilling to try VR therapy, particularly older individuals.
A larger study is underway at the hospital to measure the impact of VR therapy on the use of pain medications, length of hospital stay and post-discharge satisfaction scores.
The Pain RelieVR game was created by AppliedVR , a Los Angeles based company that is developing a variety of virtual reality content to help treat pain, depression and anxiety. Below is a promotional video released by the company.