DEA Report Downplays Role of Prescription Opioids in Drug Crisis
/By Pat Anson, PNN Editor
After a three-year absence, the DEA’s National Drug Threat Assessment (NDTA) has returned, with a tacit admission by the agency that prescription opioids don’t play much of a role anymore in the nation’s drug crisis.
Prescription opioids are mentioned only a handful of times in the 57-page report, mainly within the context of their theft and diversion declining to levels not seen in over a decade.
“The DEA Theft/Loss Reporting Database reveals that the number of unaccounted-for narcotic prescription drugs (opioids) in 2022 was at its lowest level in 12 years and continued to decline into the first nine months of 2023,” the NDTA report states.
The DEA said the number of unaccounted-for opioids fell from 19.5 million pills/units in 2011 to just 4 million in 2023, an 80% decline.
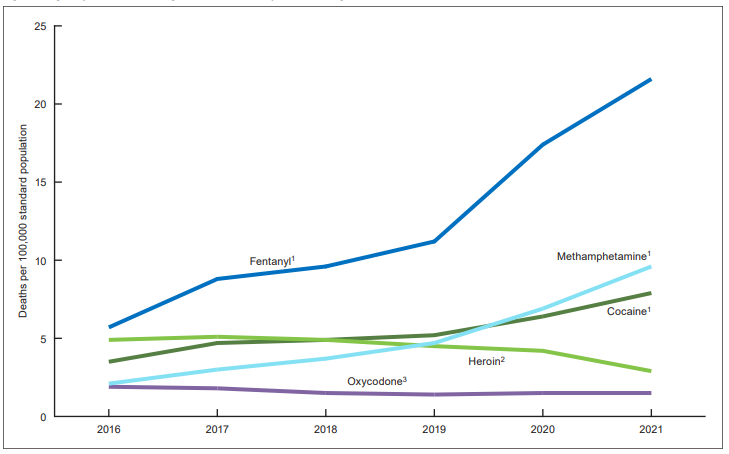
Most of the focus in the 2024 NDTA is on illicit fentanyl, methamphetamine, and counterfeit medications that have become increasingly more toxic and deadly.
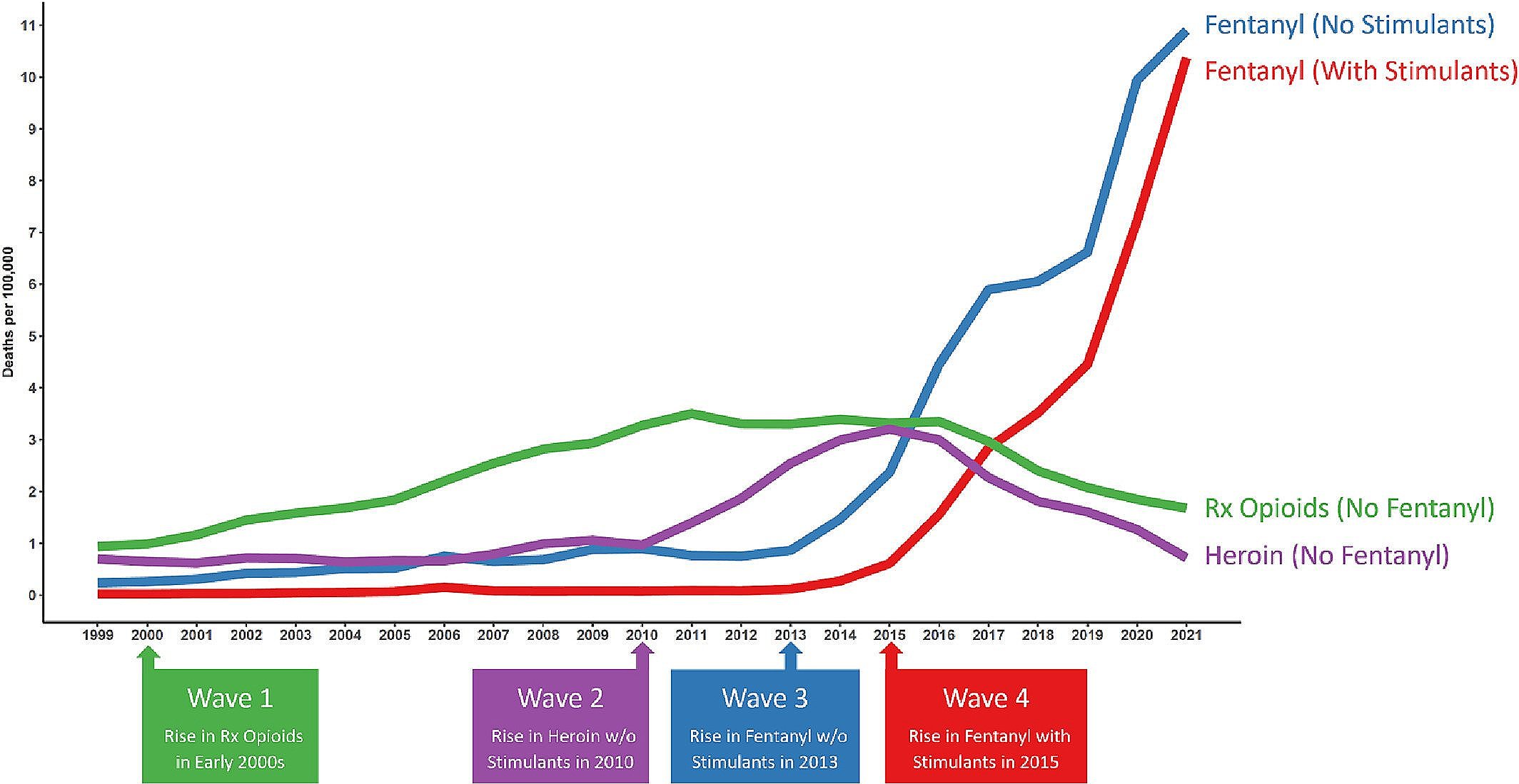
Nearly 108,000 fatal overdoses were reported in 2022, with fentanyl and other synthetic opioids – most of them illicit -- involved in 68% of drug deaths. The remaining overdoses were linked primarily to cocaine, methamphetamine and other synthetic stimulants.
“The shift from plant-based drugs, like heroin and cocaine, to synthetic, chemical-based drugs, like fentanyl and methamphetamine, has resulted in the most dangerous and deadly drug crisis the United States has ever faced,” DEA Administrator Anne Milgram said in a press release.
“At the heart of the synthetic drug crisis are the Sinaloa and Jalisco cartels and their associates, who DEA is tracking world-wide. The suppliers, manufacturers, distributors, and money launderers all play a role in the web of deliberate and calculated treachery orchestrated by these cartels.”
Most counterfeit medications in the U.S. are spiked with illicit fentanyl, a synthetic opioid 50 times more potent than heroin and 100 times stronger than morphine. In 2023, a DEA laboratory analysis found that about 70% of counterfeit pills contain at least 2 milligrams of fentanyl, a potentially deadly dose.
Fake pills are also increasingly being found with xylazine, a potent animal tranquilizer, and nitazenes, a synthetic opioid chemically unrelated to fentanyl. According to some estimates, nitazenes are 40 times more potent than fentanyl and 1,000 times more potent than morphine. Nitazenes have never been approved for medical use in the United States.
Although Milgram called the NDTA “a critical tool for informing and educating the public about the current drug threats,” the DEA’s annual report literally disappeared from public view three years ago. The last NDTA was released in 2021.
The DEA did not respond to a request for comment from PNN on why a NDTA was not published for three straight years or why one was finally released this week.
The DEA has been under growing criticism for its failure to stop fentanyl trafficking and for imposing steep cuts in production quotas on drug manufacturers, which has contributed to record shortages of opioids, ADHD stimulants and other essential drugs.
Sometimes, what is not disclosed in the DEA’s report can be just as revealing as what is. For example, while the DEA officially lists kratom as a “drug of concern” and even tried to ban the herbal supplement, the agency has never said a word about kratom in a NDTA report. Not in 2021. And not in 2024.