Lasers Work for Fibromyalgia, But Why So Pricey?
/By Ryan Baker, Guest Columnist
I’ve had severe fibromyalgia for 14 years, and I’ve been disabled as long. Without a doubt, the pain is certainly a central issue, along with the severe fatigue, flare ups, and crashes.
It’s an absolutely miserable disease that’s intrusive and destructive. I broke commitments that really shouldn’t be broken, which put a strain on personal relationships. The pain is a level of suffering that can easily push one to insanity or worse.
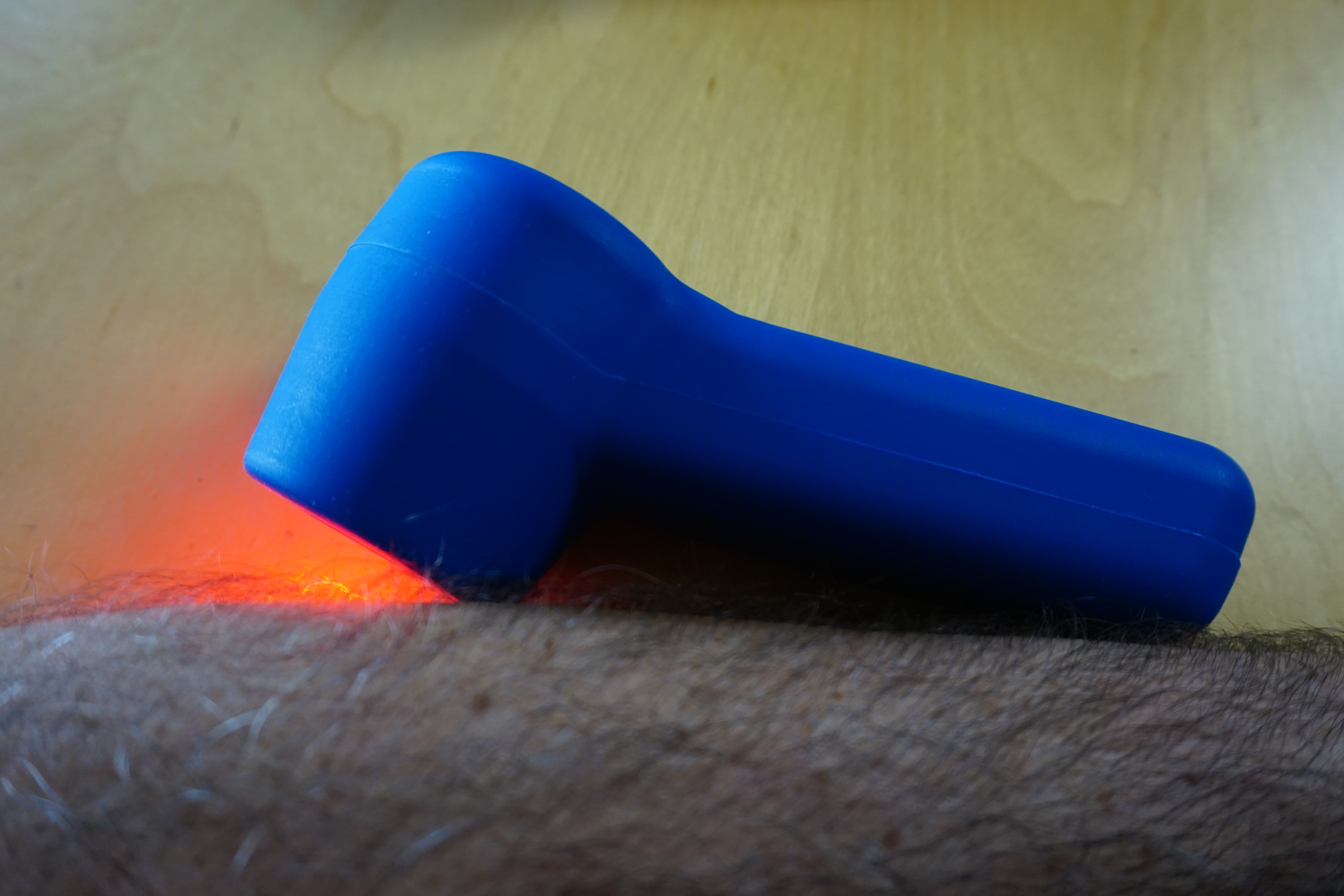
I found laser therapy last October at my chiropractor’s office, where they have a $25,000 K-Laser. While it worked great, I could not get enough coverage all over my body as often as I needed, and it was just too expensive for office visits.
I was getting good results, so I dove into trying to find a laser I could use at home, and settled on a very effective unit for $2,500. Pricey, but worth the convenience of having one I could use whenever I wanted.
Since receiving the TQ Solo laser in late January, I have not taken any prescription pain pills. My hydrocodone, methocarbamol, and Klonopin, which I had whittled down long before the laser to “emergency use only” (once every 3-7 days), have gone untouched since I’ve had the laser.
I have taken 2 ibuprofens for a dehydration headache, but no other OTC meds, aside from vitamins. I take a sleep aide and blood pressure medication, that’s it.
TQ SOLO LASER
It still astonishes me how well laser therapy works. I still suffer from fibro fog, low energy, and all of the other problems associated with fibromyalgia, but my pain levels have dropped from a constant 7-9 out of 10, to a much more tolerable 2-4. I use the laser between 20 minutes to an hour or more a day, and rather than become resistant, my body seems to respond better after getting used to treatment.
Some areas are completely free of pain at times, which hasn’t happened in 14 years, but if I stop treatment the pain returns. It’s not a cure, my fibro is still terribly limiting, but it’s an amazing treatment for the pain. The decrease in my personal suffering has been outstanding.
The laser is like an alarm clock for under active mitochondria, only stimulating the cells in need. Properly functioning tissue (not in pain) have little to no response, while damaged or inflamed tissue “wake up” and begin healing. Some areas need daily treatment, like my calves and back, while other areas can go days between treatments.
If you’re a fan of science fiction, this is the coolest thing since the smartphone made Captain Kirk’s communicator look silly.
I find the 5 hertz setting, the deepest setting, to be the most beneficial. It’s like a massage, but deeper, and there’s no pain from working tender tissue. In fact, there is very little sensation during treatment. If I can feel the treatment at all, it’s usually a mild tingle or twitch, which I consider a signal to treat more intensely.
The laser does not hurt or burn. It’s very comfortable and soothing, and treating before bed is fantastic for sleep. I don’t wake up with that stiff, poisonous feeling ache anymore.
I began researching all sorts of red light therapy. I’ve tried several, along with some LED only therapies. I even tried a heat lamp. While the heat lamp and LED therapies felt okay, they were no match for the laser.
While searching for other light therapy devices, I found the Handy Cure. It has a striking resemblance to the TQ Solo I had purchased, but it was selling for under $600. Same frequency settings, same power, same everything. Only the handle was different, as far as I could tell.
I looked it up, and it was made by the same company that makes the TQ Solo. But why so much cheaper? Was it a knock off? Was it less potent, or somehow lower quality? I put an order in.
After using the Handy Cure side by side for weeks with the TQ Solo laser, I can’t tell any difference. It’s just as effective. I’d overpaid by $2,000. I’m not wealthy, and I assume most fibro patients aren’t either, so that hurt.
I started looking into other lasers and found the Game Day laser. It looks exactly like the Handy Cure, no doubt about it, only the labels were different. Instead of variable, 50 hertz, and 5 hertz, the menu is a simple 1, 2, and 3. It appears to me that the Game Day is simply a rebadged Handy Cure.
handy cure laser (left) and TQ solo laser(right)
You’d think the Game Day would be priced more like the Handy Cure, but it’s listed for $2,995! My jaw dropped when I saw that, but the picture became crystal clear. All of these lasers had the same manufacturer and, except for subtle differences, appear to be essentially the same products.
But one sells for under $600 and the other is marked up to nearly $3,000. Why?
I’m not against the profit motive, but I am when people are suffering and treatment is unnecessarily kept out of reach.
One month later, I have become a distributor for the Handy Cure, making YouTube videos to bring laser therapy to the attention of fellow fibromyalgia patients. It’s been a big adjustment, but a meaningful one. I have no idea what I’m doing, I just know lasers work, and they take some of the “crazy” out of fibromyalgia.
Fibromyalgia pain is real and physical, not some form of hypochondria or mental illness. If it was, the laser would have no physical effect. But it works reliably for my pain, even when I’m particularly depressed.
I feel vindicated, because something finally works for the pain when powerful opiates barely made a dent. It’s not in my head.
(Editor's note: Since this article was first published, Pain News Network has been contacted by Max Kanarsky, President and CEO of Multi Radiance Medical, the maker of the Handy Cure laser. Mr. Kanarsky maintains that the "Handy Cure" featured in this article is a counterfeit reproduction of his product, is not FDA cleared, and "might present a hazard to users.")
Ryan Baker lives near Sacramento, California. You can learn more about laser therapy by visiting his website, Chronic Pain Laser.
Pain News Network invites other readers to share their stories with us. Send them to: editor@PainNewsNetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represent the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.