Pain Research Moving at Snail’s Pace
/By Pat Anson, Editor
It often seems like research into new treatments for chronic pain are moving at a snail’s pace.
That's literally the case at the University of Utah, were scientists are studying conus regius, a small marine cone snail found in the Caribbean Sea. The snail's venom is so potent that it paralyzes and kills its prey.
Researchers have isolated a compound in the snail's venom – called Rg1A4 – that has anesthetic effects that last far longer than opioid pain medication.
When injected into laboratory rats, the compound is cleared from the animal’s body in 4 hours, but its analgesic effect still works 72 hours later.
The duration of that pain relieving effect suggests that Rg1A4 has a restorative effect on some components of the nervous system.
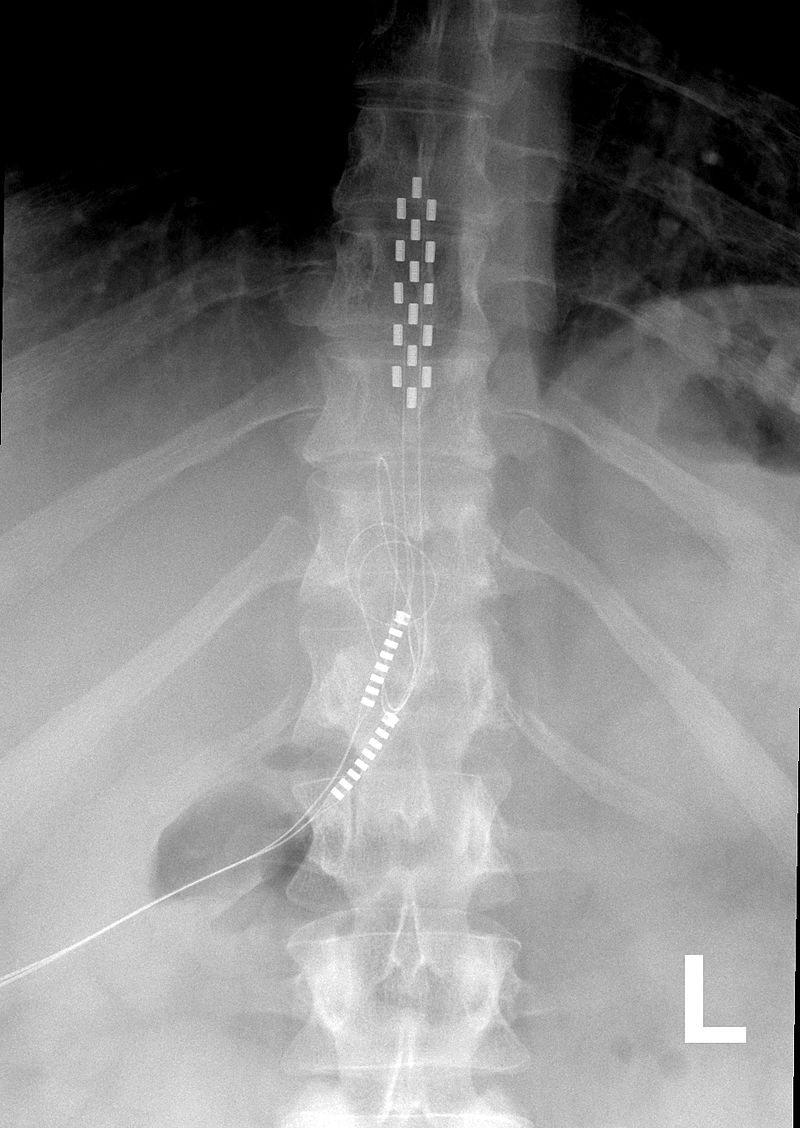
UNIVERSITY OF UTAH PHOTO
"What is particularly exciting about these results is the aspect of prevention," said J. Michael McIntosh, MD, a professor of psychiatry at the University of Utah Health Sciences. "Once chronic pain has developed, it is difficult to treat. This compound offers a potential new pathway to prevent pain from developing in the first place and offer a new therapy to patients who have run out of options."
Most pain medications available today work through a limited number of neural pathways and are not sufficient to completely alleviate chronic pain. Opioids also have risky side effects, such as addiction and respiratory depression.
"RgIA4 works by an entirely new pathway, which opens the door for new opportunities to treat pain," said McIntosh. "We feel that drugs that work by this pathway may reduce burden of opioid use."
Researchers around the world are studying the potential medical benefits of cone snail venom. In addition to its analgesic effects, German scientists have found that peptides in the venom decompose quickly and are unlikely to cause dependency.
A pharmaceutical drug derived from cone snails has already been developed and is marketed under the brand name Prialt. The drug is injected in spinal cord fluid to treat severe pain caused by failed back surgery, injury, AIDS, and cancer.