Committees Support CDC Opioid Guidelines
/By Pat Anson, Editor
Two advisory committees expressed broad support Thursday for the controversial guidelines for opioid prescribing being developed by the Centers for Disease Control and Prevention (CDC). Those guidelines discourage primary care physicians from prescribing opioids for chronic non-cancer pain and recommend other therapies such as over-the-counter pain relievers, acupuncture, and cognitive behavioral therapy.
One newly formed committee --- which the CDC calls a “workgroup” --- did express “significant concern” about the cost of those alternative pain therapies and whether they are covered by insurance. The workgroup's report to the CDC’s Board of Scientific Counselors (BSC) also suggested that the guidelines be “framed with positive rather than negative language” that supports “integrated care for people with chronic pain.” It also recommends the impact of the guidelines be monitored for “unintended consequences” after they are implemented.
The BSC voted to support the workgroup’s report, which can be found here.
“The BSC voted unanimously: to support the observations made by the BSC Opioid Guideline Workgroup; that CDC adopt the guideline recommendations that, according to the workgroup’s observations, had unanimous or majority support; and that CDC further consider the guideline recommendations for which the workgroup had mixed opinions,” said CDC spokesperson Courtney Leland in an email to Pain News Network.
“CDC is taking the BSC’s recommendations, as well as comments received from the public, into consideration in revising the guideline. The guideline is a priority for our agency. Given the lives lost and impacted every day, we have an acute sense of urgency to issue guidance quickly.”
The CDC planned to implement the guidelines this month with little public input, but was forced to change course after widespread criticism about its secrecy and lack of transparency during the drafting of the guidelines. In response to critics, the 10-member workgroup was formed three weeks ago and met four times by teleconference to review the guidelines. A potential legal problem for the CDC is that none of the workgroup’s meetings were open to the public. The workgroup also reviewed the guidelines with outside consultants without publicly disclosing who they were.
The Washington Legal Foundation (WLF) has threatened to sue the agency for its “culture of secrecy” and “blatant violations” of the Federal Advisory Committee Act (FACA), which requires meetings to be open to the public.
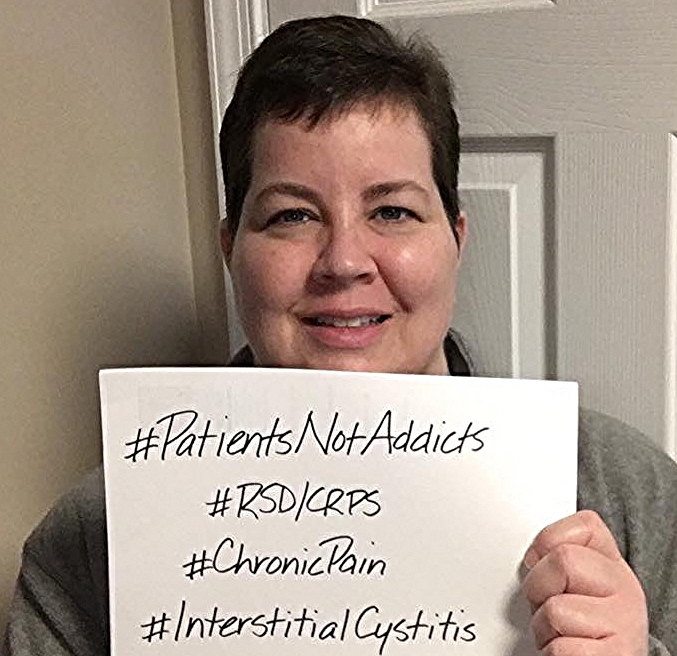
Over 4,300 online comments were received by CDC during a public comment period that ended earlier this month. Many opposed the guidelines as being too restrictive, while others wished the guidelines were stronger to combat the so-called epidemic of opioid abuse and overdoses. There were passionate arguments on both sides, but in the end the workgroup decided that the case for the guidelines was stronger.
“Comments from patients and family members, in particular, expressed the desire that patient-centered care is enhanced rather reduced by these Guidelines. Members felt that the guidelines could be implemented in a manner consistent with patient centered care,” the workgroup said in its report.
As many as 11 million Americans use opioids for long-term chronic pain and many fear losing access to the drugs if the guidelines are adopted.
“The purpose of the guideline is to help to primary care providers offer safer, more effective care for patients with chronic pain and to help reduce opioid abuse disorder and overdose from these drugs,” said Debra Houry, MD, director of the CDC’s National Center for Injury Prevention and Control, which is overseeing development of the guidelines.
"The guideline itself is not a rule, regulation or law. It is not intended to deny access to opioid pain medication as an option in pain management. It is not intended to take away physician discretion and decision making.”
“Pain specialists and their patients fear the Guidelines will not be used that way though and adoption by boards, professional organizations, and insurers will pressure even specialty pain providers to taper patients,” said Anne Fuqua, a chronic pain sufferer and patient advocate. “Pain patients nationwide have been experiencing dose reductions and losing access to care altogether for several years, with the situation becoming more acute in the past year. In an environment where physicians are tapering patient doses or ceasing opioid prescribing altogether, I feel these guidelines will serve like an accelerant in a growing fire.”
Although the CDC has said it doesn’t want the guidelines implemented until they are finalized, Fuqua said many doctors are already doing just that. She said her faith in democracy “took a swift kick in the teeth” as she listened to the workgroup’s presentation during a conference call. Fuqua was not given an opportunity to speak, although the president and founder of Physicians for Responsible Opioids Prescribing (PROP) were given time to address the BSC in support of the guidelines they helped draft.
“There were 28 comments supporting the Guidelines and 4 dissenters. One physician made statements partially supportive of our needs. CDC will no doubt use this ‘overwhelming support’ to justify adoption of the guidelines. I fear they see us as simply a casualty of war, much like those with tuberculosis who were quarantined to prevent disease spread. The only difference is that harming us doesn't save other lives,” she said.
CDC has not released a timetable on when it plans to finalize or implement the guidelines.