All Forms of Medical Marijuana Now Legal in Canada
/By Pat Anson, Editor
Medical marijuana advocates are cheering – and some health officials are jeering – a landmark ruling by the Supreme Court of Canada allowing patients to use cannabis in any form they choose.
The unanimous decision greatly expands the use of medical marijuana in Canada beyond the traditional means of smoking it – to include everything from cookies and teas to ointments and tinctures that are laced with THC and cannabinoids, marijuana’s active ingredients.
Many users believe smoking marijuana is harmful to their health. But under Canada’s Controlled Drug and Substances Act, use of marijuana outside of its “dried” form could result in possession and drug trafficking charges.
That’s what happened to Owen Smith, a baker for the Victoria Cannabis Buyers Club, who was arrested in 2009 for making over 200 cookies containing marijuana, as well as various oils and lotions.
The Supreme Court upheld two lower court decisions that acquitted Smith, saying the government’s marijuana law violated his right to liberty and security "in a manner that is arbitrary and hence is not in accord with the principles of fundamental justice."
The court declared the marijuana section of the law “null and void” immediately, rather than give Parliament a chance to rewrite it. To do otherwise, the court said, would "leave patients without lawful medical treatment.”
"I'm proud and really happy today for all those people who are going to benefit from this ruling," Smith said at a press conference in Victoria, British Columbia. “Across the country there will be a lot more smiles and a lot less pain.”
“How exciting is this! I am thrilled with this decision,” said Ellen Lenox Smith, a medical marijuana advocate and columnist for Pain New Network.
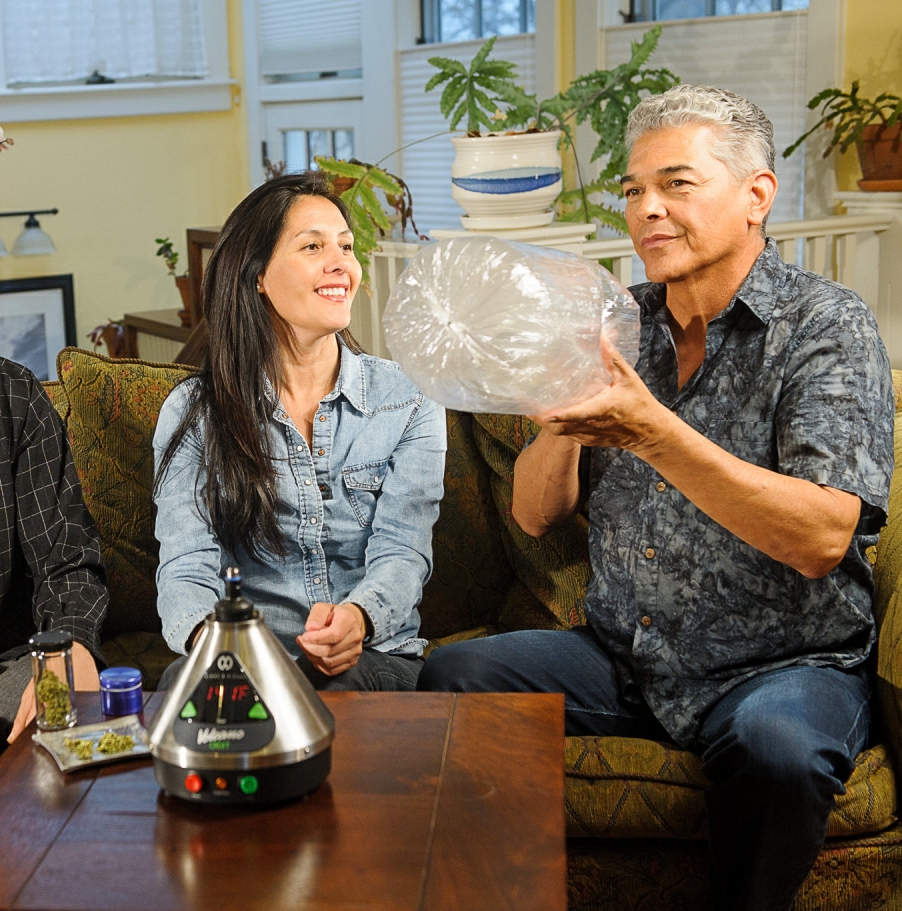
Smith, who is not able to smoke marijuana because of a medical condition, wrote a column earlier this month about ways to consume marijuana for pain relief without smoking it. She prefers a nightly dose of a marijuana oil that she makes herself.
“It all depends on the patient, condition, type of medicine used and how your body reacts. This is a wonderful alternative. We all have to find the magical way to administer,” she said. “I applaud them for having the courage to understand the reality of this medication. One size does not fit all and allowing for the variety is wonderful and something I hope we will always be allowed to turn to for help.”
Canadian health officials are angry about the court’s decision.
"Frankly, I'm outraged by the Supreme Court," said Health Minister Rona Ambrose, according to CBC News.
"Let's remember, there's only one authority in Canada that has the authority and the expertise to make a drug into a medicine and that's Health Canada," she said. "Marijuana has never gone through the regulatory approval process at Health Canada, which of course, requires a rigorous safety review and clinical trials with scientific evidence."
Ambrose said the government would fight against the court's "normalization" of marijuana with a public relations campaign outside the courtroom.
"We will continue to combat it. We will continue our anti-drug strategy, we will target youth with the message that marijuana pot is bad for them," the minister said. "We'll continue to work with medical authorities across the country to make sure they're involved in the message."
British Columbia’s chief medical health officer says edible marijuana products should come with labels listing the strains used and their potency, to help ensure that users don’t accidentally overdose and get sick.
“Quality control, certainly for medical use, should be labelled and analyzed,” Dr. Perry Kendall told the Vancouver Sun. “It would be better for people, if they’re taking an illegal product by mouth, to know how much and what, is in it.
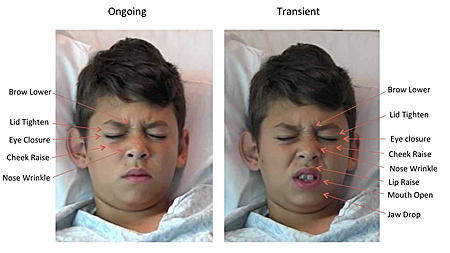
“It can take a half an hour to an hour to absorb through the stomach. If you’re a naive young user you might go on eating and eating because you don’t feel anything and then you take more than you want to.”
Medical marijuana – in all its various forms -- is legal in 23 U.S. states and the District of Columbia. However, there are no regulations governing its quality, dosage or labeling.
“Evidence in the U.S. is that wider availability of these products is causing increased poisonings in children, and we want to prevent this from occurring here in Vancouver,” the city of Vancouver warned in a news release after the Supreme Court’s ruling. “Unregulated edible products also pose a greater risk to adults than other forms of marijuana.”