FDA Approves New Opioid Film Patch
/By Pat Anson, Editor
The U.S. Food and Drug Administration has approved a new delivery system for the treatment of chronic pain – the first of its kind to use an oral film patch containing buprenorphine.
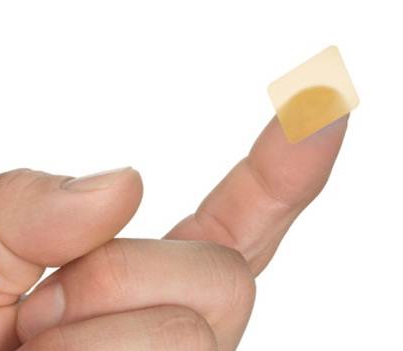
The film patch – which will be sold under the brand name Belbuca -- was jointly developed by Endo International (NASDAQ: ENDP) and BioDelivery Sciences (NASDAQ: BDSI). It’s expected to become available early next year.
image courtesy biodelivery sciences
Belbuca is designed to dissolve in the mouth, delivering buprenorphine through the inside lining of the cheek and into the bloodstream faster than conventional pills or skin patches. Buprenorphine is a weaker acting opioid that has long been used to treat both addiction and chronic pain.
“Belbuca provides a unique approach for chronic pain management, combining the proven efficacy and established safety of buprenorphine with a novel buccal film delivery system that adds convenience and flexibility," said Richard Rauck, MD, Director of Carolinas Pain Institute in Winston Salem, NC.
"For both opioid-naïve and opioid-experienced patients who require around-the-clock treatment and for whom alternative treatment options are inadequate, Belbuca offers appropriate, consistent pain relief and a low incidence of typical opioid-like side effects.”
Because the film delivers buprenorphine into the bloodstream faster than conventional methods, lower doses are needed to treat pain. Belbuca will be available in seven different dosage strengths, allowing for flexible dosing every 12 hours.
FDA approval of Belbuca was based on two Phase III studies involving over 1,500 patients with moderate to severe chronic low back pain. Patients who used Belbuca reported “statistically significant improvement” in pain relief over a 12-week period, compared to a placebo. The most common adverse reactions to Belbuca were nausea, constipation, headache, vomiting, fatigue, dizziness, somnolence, diarrhea, dry mouth, and upper respiratory tract infection.
Buprenorphine is a Schedule III controlled substance, which means it has a lower abuse potential than many other opioids. It may also be easier to get a prescription for than Schedule II drugs such as hydrocodone.
“If you’re going to use an opioid, I think based on its classification, Belbuca really does offer some significant benefits,” said Dr. Mark Sirgo, President and CEO of BioDeliversy Sciences.
“There are two areas this product will be used for. Those that are stepping up from a Motrin-like drug, a non-steroidal anti-inflammatory, that no longer controls their chronic pain. Those are good candidates for Belbuca. And in those that may already be on a Schedule II product such as Vicodon, one of the oxycodone products or morphine products, where a physician may feel more comfortable using a buprenorphine product than a Schedule II opioid."
Sirgo says Belbuca is also less likely to abused than a pill, because the film patches are difficult to grind or liquefy for snorting or injecting.