‘Chili Pepper’ Patch Works Better Than Lyrica
/By Pat Anson, Editor
A skin patch containing a synthetic substance found in chili peppers works better than pregabalin in treating patients with neuropathic pain, according to the results of a new study conducted in Europe.
Pregabalin is the generic name for Lyrica, a medication made by Pfizer that is widely prescribed for neuropathy, fibromyalgia and other chronic pain conditions.
Nearly 660 adults with moderate to serve peripheral neuropathic pain (PPN) caused by shingles were randomly assigned to groups receiving either a single treatment with the Qutenza patch or a daily dose of pregabalin.
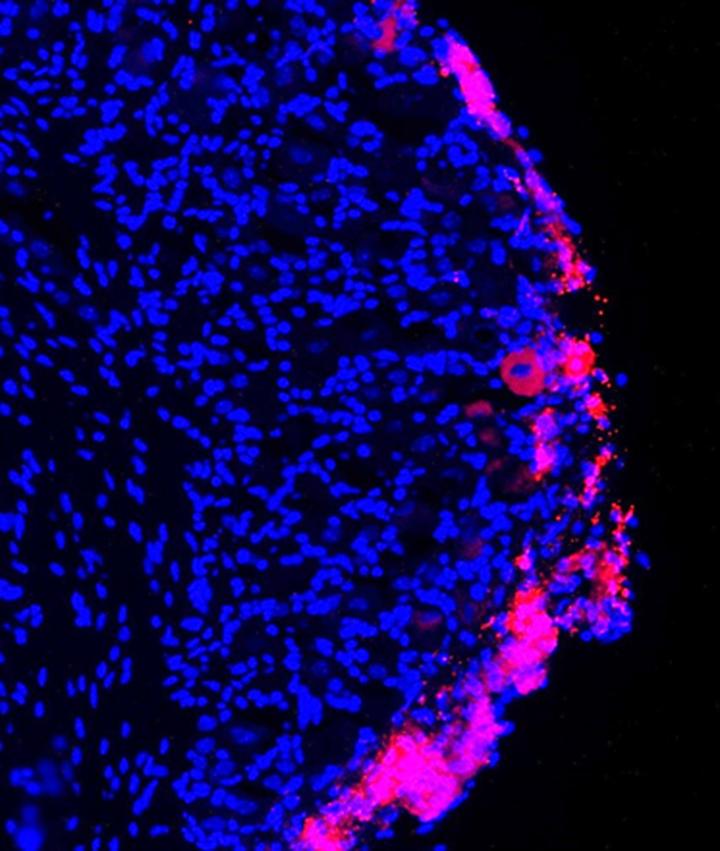
The 8% capsaicin patch uses a synthetic form of capsaicin, the substance that gives chili peppers their heat, to dull pain-sensing nerves in the skin.
By the 8th week of the study, a little over half of the patients in both groups had achieved pain relief of at least 30 percent. However, the median time to pain relief in the capsaicin group was 7.5 days, compared to 36 days in the pregabalin group. Those who used the Qutenza patch were also more satisfied with their treatment and had fewer side effects.
The study, which is published in the European Journal of Pain, was funded by Astellas Pharma Europe Ltd., which makes the Qutenza patch.
"This is an important and well-conducted study that was designed to mimic everyday practice, allowing those patients randomised to the pregabalin arm to be individually titrated to the optimal tolerated dose,” said lead investigator Maija Haanpää, a professor in the Department of Neurosurgery at Helsinki University in Finland. “We found that topical treatment with the capsaicin 8% patch was non-inferior to the current standard of care. This means that there is now another treatment option for people with peripheral neuropathic pain, especially those patients who are very sensitive to the side effects of systemic medication or for those who do not wish to take tablets every day."
Until now, no head-to-head clinical trials have directly compared the capsaicin patch to pregabalin or other treatments for PNP.
"There is a need to tailor treatment to individual patients and these data show that the capsaicin 8% patch is an efficacious agent to manage patients with peripheral neuropathic pain," said Dr. Andreas Karas, Senior Director, Medical Affairs for Astellas Pharma.
In September of this year, the European Commission approved a label extension for Qutenza to include diabetic patients with neuropathic pain. In the United States, Qutenza has only been approved by the FDA for the management of neuropathic pain associated with postherpetic neuralgia.
Neuropathic pain is characterized by tingling pain that develops as a result of nerve damage caused by conditions such as shingles, diabetes, amputation, inflammation, and cancer. About 8% of adults worldwide suffer from neuropathy. Many drugs used to treat neuropathic pain, such as Neurontin and Lyrica, often don’t work or have unpleasant side effects. Common side effects of Lyrica are dizziness, nausea, headache, weight gain and fatigue.
In addition to neuropathic pain, Lyrica is approved by the FDA to treat chronic pain associated with fibromyalgia, epilepsy, shingles, diabetic peripheral neuropathy, and spinal cord injury. The drug is also prescribed “off label” to treat lumbar spinal stenosis, the most common type of lower back pain in older adults.
Lyrica is Pfizer’s top selling drug with annual worldwide sales of over $5 billion.