How Curcumin Helped My Chronic Pain
/By Judie Plumley, Guest Columnist
In 2013 I had a spinal fusion, 7 months after I had transvaginal mesh removal and reconstruction surgery. During the operation, I contracted a severe bacterial infection in my spine called methicillin-resistant Staphylococcus aureus (MRSA).
To make a long, painful story short, I ended up having 5 more spinal surgeries in the next year. They did not get rid of the infection until it had liquefied 2 vertebrae and surrounding tissue. It almost killed me.
There is extensive nerve damage, and my back is filled with rods and screws.
During the worst of it I was on fentanyl, Dilaudid, Demerol, gabapentin (Neurontin) and oxycodone. I spent 2015 weaning myself off the narcotics. I was losing my insurance and I knew if I didn't, I would be in a withdrawal from hell.
I did go to two pain clinics, but just simply refused to be treated like a criminal. I started exploring other options to deal with my pain.
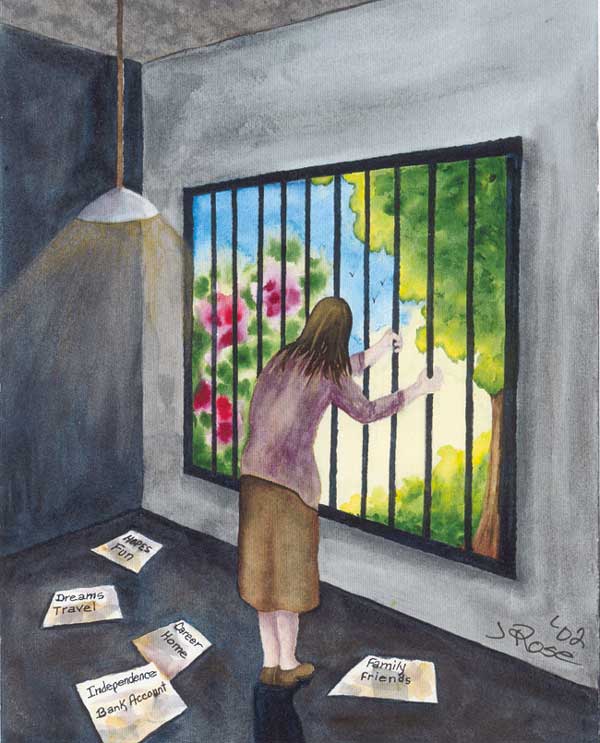
Judie Plumley's spine
Since my son is a massage therapist, the first thing I started as soon as I was able was to get weekly massages while I healed. Joseph stretched the forming scar tissue in order to allow me to move.
Next, I started using kratom, a half teaspoon twice a day. I was amazed by the effect. It knocked out a considerable amount of pain, but I was still spending 12 to 14 hours in bed each day.
About 2 months ago, my sister told me to try a supplement that combined curcumin – a yellow spice -- with black pepper oil. I bought it from Amazon, $15 for 120 caps.
I am amazed with the results! My pain is now bearable. I can do about twice as much as I could before, and I am spending much less time in bed.
I am now in the process of getting off the gabapentin, but it is much harder than any of the narcotics. The withdrawal is horrible. As soon as this devil is off my back, I am done with doctors and hospitals.
curcumin
I refuse to be treated like a drug addict or a criminal. I believe pain clinics are nothing more than a scam and that drug companies intentionally add things to their drugs to make people addicted. The antidepressants that are taking the place of opiates are even worse! Ever heard of a brain zap?
I swear, they are trying to kill us, or drive us to kill ourselves. I don't understand why they are attacking people in chronic pain. It's a terrible way to live. I am lucky I have my son, a good support system, and have found something that works. Life is hard enough as it is.
I have kept a journal since 2014. I plan to write a book about my experience with MRSA. Unless you’ve had it, you have no idea how dangerous and painful it is.
Judie Tucker Plumley lives in Georgia.
Pain News Network invites other readers to share their stories with us. Send them to: editor@PainNewsNetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.