Migraine Drugs No More Effective Than Placebo for Kids
/By Pat Anson, Editor
Two medications commonly prescribed to prevent migraines in adults are no more effective than a placebo when given to children and teenagers, according to a new study published in The New England Journal of Medicine.
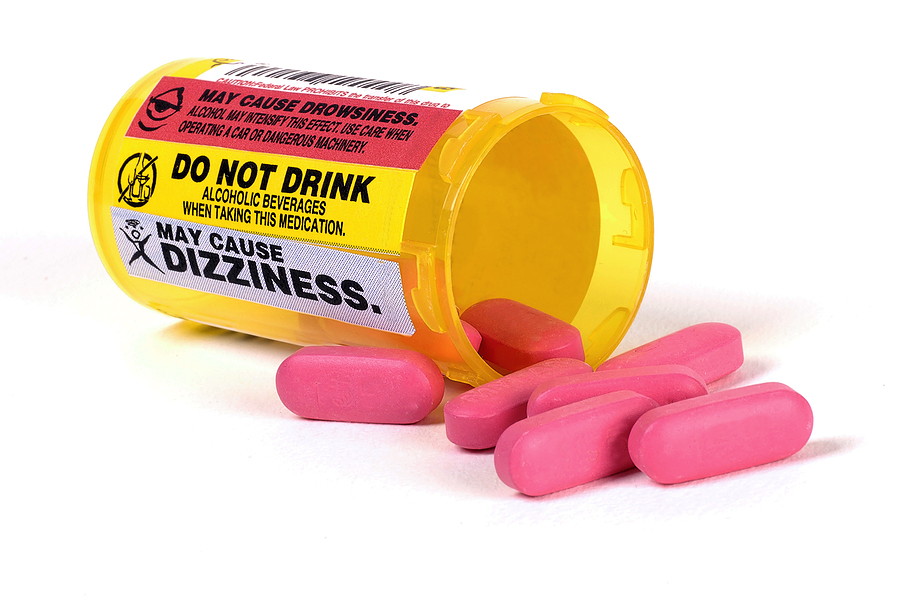
Researchers affiliated with the Childhood and Adolescent Migraine Prevention (CHAMP) study randomly assigned 328 children and adolescents into three groups. One group received a daily dose of amitriptyline (Elavil), the second group received topiramate (Topamax), and the third group was given an ordinary sugar pill.
After 24 weeks, 52 percent of those taking amitriptyline and 55 percent of those taking topiramate had a 50 percent or more reduction in the number of headache days.
But the sugar pill was more effective, with 61% of the placebo group reporting their number of headache days reduced by 50 percent or more.
Researchers say the expectation of responding to a medication may have surpassed the pharmacological effects of taking a drug.
"The study was intended to demonstrate which of the commonly used preventive medications in migraine was the most effective. What we found is that we could prevent these headaches with either a medication or a placebo," says Andrew Hershey, MD, co-director of the Cincinnati Children's Headache Center and senior author of the study. "This study suggests that a multi-disciplinary approach and the expectation of response is the most important, not necessarily the prescription provided."
The children taking amitriptyline or topiramate had a significantly higher rate of side effects, including fatigue, dry mouth and, in three cases, mood alteration. About a third of those taking topiramate had paresthesia, a "pins and needles" tingling sensation in their hands, arms, legs or feet.
"The interpretation of these results is very challenging. In most situations, trials that fail to show benefit of an intervention do so because study participants do not improve. That was not the situation here. A majority of all study participants improved, regardless of their assigned treatment group," says Chris Coffey, PhD, a professor of biostatistics in the University of Iowa's College of Public Health, who was lead statistician for the study.
Researchers say further studies are needed identify the best ways to treat pediatric migraines. Simply prescribing sugar pill would be unethical without the patient’s knowledge.
"Our national team was hoping to develop evidence to drive the choice by medical providers of the first line prevention medication for helping youth with migraine, but the data showed otherwise, says Scott Powers, PhD, a pediatric psychologist and co-director of the headache center at Cincinnati Children's.
"We see this as an important opportunity for health care providers, scientists, children, and families because our findings suggest a paradigm shift. First line prevention treatment will involve a multidisciplinary team approach and focus on non-pharmacological aspects of care."
One of the non-pharmacological therapies being used is cognitive behavior therapy (CBT). While CBT has not been directly compared to a placebo for pediatric migraines, neurologists and psychologists say it can be a helpful component in pain care.
As many as one out of five teens suffers from migraines, but treatment options are limited compared to adults. Last year the Food and Drug Administration approved two new treatments for pediatric migraine. Zonig is a nasal spray that provides pain relief in as little as 15 minutes, while Treximet is a medication that contains sumatriptan and naproxen, a non-steroidal anti-inflammatory drug (NSAID). Both Zonig and Treximet have been available for years to treat adult migraine.
Migraine is thought to affect a billion people worldwide and about 31 million Americans adults. In addition to headache pain and nausea, migraine can also cause vomiting, blurriness or visual disturbances, and sensitivity to light and sound. About half of people living with migraine are undiagnosed.