Trump Administration Promises Relief to Patients
/By Pat Anson, Editor
A spokesman for the Trump administration pledged this week that the Department of Health and Human Services (HHS) would provide relief to patients who are "being harmed by the status quo.”
Matt Lloyd, a former top aide to Vice President Mike Pence, recently assumed the job of chief spokesman for HHS, the federal department that oversees the Food and Drug Administration, the Centers for Disease Control and Prevention, and the Centers for Medicare and Medicaid Services (CMS).
Lloyd made his comment in an unusual statement emailed to reporters after CMS released a report Friday that showed the number of Americans who signed up for insurance during Obamacare’s annual enrollment period had fallen to 9.2 million. That’s down from 9.6 million the year before.
“Obamacare has failed the American people, with one broken promise after another. As noted in the report today from CMS, premiums in the ACA marketplace have increased 25 percent while the number of insurers has declined 28 percent over the past year,” Lloyd said.
MATT LLOYD
“We look forward to providing relief to those who are being harmed by the status quo and pursuing patient-centered solutions that will work for the American people.”
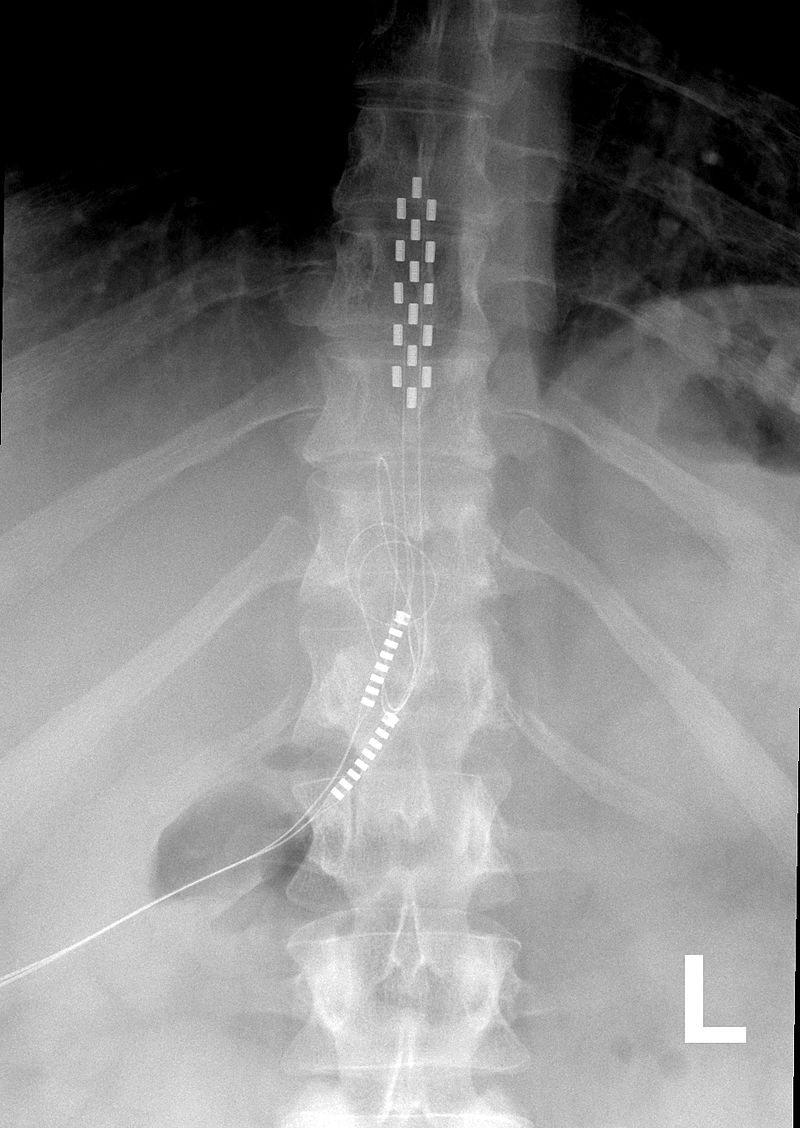
Ironically, Lloyd made his statement two days after CMS invited public comment on the agency’s plans to have Medicare adopt the CDC’s opioid prescribing guidelines – a move that could affect thousands of patients who use opioids for pain relief. The CDC guidelines are voluntary and only intended for primary care physicians, but CMS wants to apply them to all doctors who prescribe opioids for non-cancer pain. A strict daily limit on opioids would also be set at 90 mg of a morphine equivalent dose.
Doctors and patients who don’t follow the proposed CMS policy could face punitive action, such as being dropped from Medicare coverage and insurance networks. CMS has estimated that over 15,000 Medicare beneficiaries who receive high doses of opioids for pain relief could be impacted
CMS contracts with dozens of private insurance companies to provide health coverage to about 54 million Americans through Medicare.
The agency’s “Opioid Misuse Strategy” was developed during the final months of the Obama administration, but could be quickly adopted by the new administration. CMS is only accepting public comments on its proposals until March 3 and plans to publish the final rules by Monday, April 3, 2017.
Comments on the CMS rule change should be mailed to: AdvanceNotice2018@cms.hhs.gov.
Comments can be emailed to Matt Lloyd at: Matt.Lloyd@hhs.gov.