Limits on Rx Opioids Led to Unintended Consequences in Australia
/By Pat Anson
An Australian study highlights some of the benefits and unintended consequences of efforts to limit the prescribing of opioid pain medication.
Like the United States, there’s been a fair amount of controversy in Australia about opioid medication and the role it played in the so-called opioid crisis. In response, Australian regulator took two steps in 2020 to limit prescribing: creating prescription drug monitoring programs (PDMPs), and limiting the amount of opioids and repeat prescriptions subsidized by the government.
To see how well the changes worked, researchers analyzed emergency department (ED) visits by patients prescribed opioids by primary care doctors in Victoria, the second most-populated state in Australia with over seven million people. Victoria was the first state to adopt a mandatory PDMP, which doesn’t stop a doctor from prescribing opioids but alerts them to possible misuse by a patient.
The research findings, published in the Medical Journal of Australia, show that ED visits by patients on prescription opioids fell by 11.8 visits per 100,000 people after opioids restrictions were implemented. At the same time, however, researchers identified a short-term but statistically significant increase of 7.3 ED visits per 100,000 people that were linked to non‐opioid substances.
The study didn’t identify what those non-opioid substances were, but researchers suspect that some were uncontrolled medications, such as pregabalin and antidepressants, which are often prescribed as alternatives to opioids for pain relief.
“As we expected, the new policies were associated with reduced opioid‐related harm; the reduced availability of prescription opioids presumably explains this change. We also expected that the changes would have unintended effects, and found an immediate increase in the non‐opioid substance‐related ED presentation rate that was greater among people prescribed opioids than in the control group,” researchers reported.
“One possible mechanism underlying the increase in non‐opioid substance‐related harms could be related to increased prescribing of unmonitored pain medicines, such as pregabalin and tricyclic antidepressants, following the introduction of the prescription drug monitoring program.”
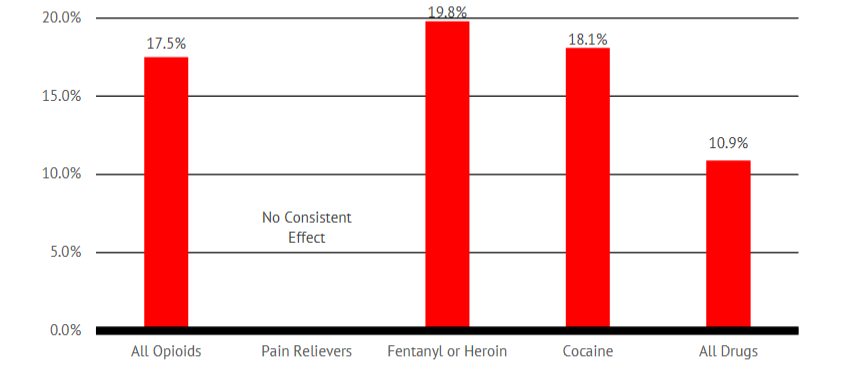
PDMPs have also had unintended consequences in the United States. In a 2021 study, the Reason Foundation found that opioid prescribing declined in states that adopted PDMPs, but that overdoses involving heroin, illicit fentanyl and cocaine significantly increased – suggesting that some patients were substituting illicit drugs for prescription opioids.
The focus on prescription opioids may have been misplaced in Victoria. According to a 2023 report by the state’s coroner, the anti-anxiety medication diazepam was the lead drug involved in fatal overdoses (213 deaths) in Victoria, followed by heroin (204 deaths), methamphetamine (164 deaths), alcohol (153 deaths) and pregabalin (78 deaths). In contrast, oxycodone was involved in 41 deaths and codeine in 24 deaths.