Feds Withdrew Request to Ban Kratom in 2018
/By Pat Anson, PNN Editor
Federal health officials quietly withdrew their request for kratom to be classified as a Schedule I controlled substance in August 2018, according to a previously undisclosed letter to the U.S. Drug Enforcement Administration.
The letter from Brett Girior, MD, Assistant Secretary for Health & Human Services (HHS), to the DEA’s acting administrator cited concerns that “there is a significant risk of immediate adverse public health consequences to potentially millions of users if kratom or its components are included in Schedule I.”
Kratom is an herbal supplement comes from the leaves of a tree that grows in southeast Asia, where kratom has been used for centuries as a natural stimulant and pain reliever. In recent years, millions of Americans have discovered kratom, using it to self-treat their chronic pain, anxiety, depression and addiction. Classifying kratom’s two active ingredients, the alkaloids mitragynine and 7-hydroxymitragynine, as Schedule I substances would effectively ban kratom by making its sale and possession illegal.
The 2018 letter from HHS was made public this week by the American Kratom Association (AKA), an advocacy group for kratom consumers and vendors, which said it obtained the letter from Rep. Mark Pocan (D-WI).
“The decision by the FDA to not disclose the recission of their recommendation for scheduling of kratom that took place more than 2 ½ years ago has significantly misled policy makers, the media, and kratom consumers in the belief a scheduling decision was imminent,” Mac Haddow, Senior Fellow on Public Policy for the AKA, said in a statement. “Six states were duped by this messaging to pass bans on kratom sales, and a number of local county and city governments also based their bans on the FDA’s claims.
“Through all of this the FDA has remained silent and has failed to disclose that HHS reviewed their scheduling recommendation and took the unprecedented action to rescind the recommendation because the FDA had failed to meet its burden under the CSA (Controlled Substance Act).”
An FDA spokesperson said it was not up the agency to disclose the letter’s existence.
“While the FDA is an agency within HHS, the letter at issue was not the FDA’s to publicly disclose and any announcement regarding a decision to schedule or not schedule a potential controlled substance is made by the Drug Enforcement Administration, not the FDA,” the spokesperson said in an email to PNN.
‘Lack of Evidence’ Kratom is Harmful
Girior’s letter to DEA said there was a “relative lack of evidence” that kratom can be abused and posed a public health threat.
“Although there remains cause for concern for 7-hydroxymitragynine and potentially mitragynine, the level of scientific data and analysis presented by the FDA and available in the literature do not meet the criteria for inclusion of kratom or its chemical components in Schedule I of the CSA at this time,” Girior wrote.
“There is still debate among reputable scientists over whether kratom by itself is associated with fatal overdoses. Further analysis and public input regarding kratom and its chemical components are needed before any scheduling should be undertaken.”
The DEA tried unsuccessfully to list kratom as a Schedule I substance in 2016, calling it an “imminent hazard to public safety,” a decision that was reversed after a public outcry from kratom supporters.
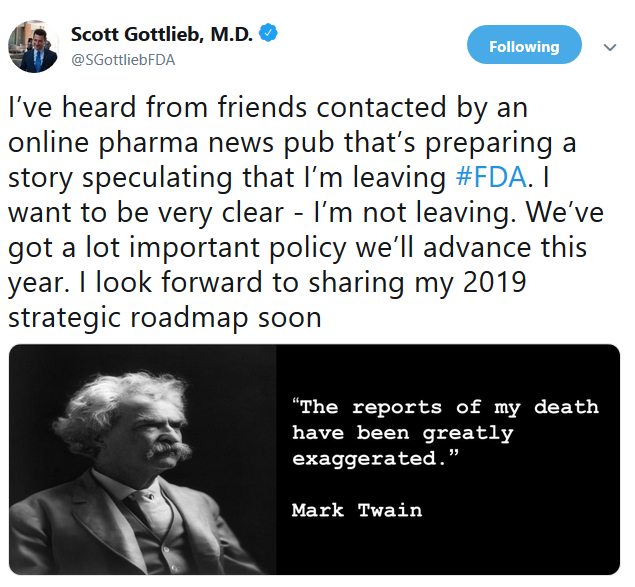
But federal efforts to demonize kratom continue to this day, led for a time by FDA Commissioner Scott Gottlieb, who claimed kratom was an opioid and should not be used to treat any medical condition. Gottlieb resigned as FDA Commissioner in 2019, eight months after Girior’s letter. The agency he led remains opposed to kratom.
“Kratom products have been associated with significant potential safety concerns. While it is important to gather more evidence, data suggest that certain substances in kratom have opioid properties that expose users to the risks of addiction, abuse and dependence,” the FDA spokesperson said.
“There is no FDA-approved drug containing, or derived from kratom, and the agency has received concerning reports about the safety of kratom. The FDA is actively evaluating available scientific information on this issue. In addition, FDA has sent numerous letters to firms that have marketed kratom products with unsubstantiated claims that their products can treat opioid withdrawal and addiction and other serious medical conditions.”
Kratom use has been growing in the U.S. as people seek alternatives to opioid pain relievers and other pharmaceutical drugs. Most kratom users say the leaves have a mild analgesic and stimulative effect, similar to coffee.
A recent study funded by the National Institute on Drug Abuse concluded that kratom is an effective treatment for pain, helps users reduce their use of opioids, and is “relatively safe” to use.