DEA: U.S. Facing ‘Fentanyl Crisis’
/By Pat Anson, Editor
The United States is facing an unprecedented “fentanyl crisis” that is likely to grow worse as drug dealers ramp up production of counterfeit pain medication made with illicit fentanyl, according to a new report from the Drug Enforcement Administration.
Fentanyl is a synthetic opioid 50 to 100 times more potent than morphine. It is legally prescribed in patches and lozenges to treat severe chronic pain, but illicit fentanyl has recently emerged as a fast-growing scourge on the black market, where it is increasingly being used in the manufacture of counterfeit drugs.
“The counterfeit pills often closely resemble the authentic medications they were designed to mimic, and the presence of fentanyls is only detected upon laboratory analysis,” the DEA warns in the unclassified report.
“Fentanyls will continue to appear in counterfeit opioid medications and will likely appear in a variety of non-opiate drugs as traffickers seek to expand the market in search of higher profits. Overdoses and deaths from counterfeit drugs containing fentanyls will increase as users continue to inaccurately dose themselves with imitation medications.”
Dozens of Americans have died this year after ingesting counterfeit versions of oxycodone, Norco and Xanax, which are virtually indistinguishable from the real medications. Even a few milligrams of fentanyl can be fatal.
Tennessee bureau of investigation
The DEA said “hundreds of thousands of counterfeit prescription drugs” laced with fentanyl were on the market and predicted more would be produced because of heavy demand and the “enormous profit potential” of fake medication.
“The seizures of fentanyl-laced pills and clandestine pill press operations all across North America indicate that this is becoming a trend, not a series of isolated incidents,” the DEA said.
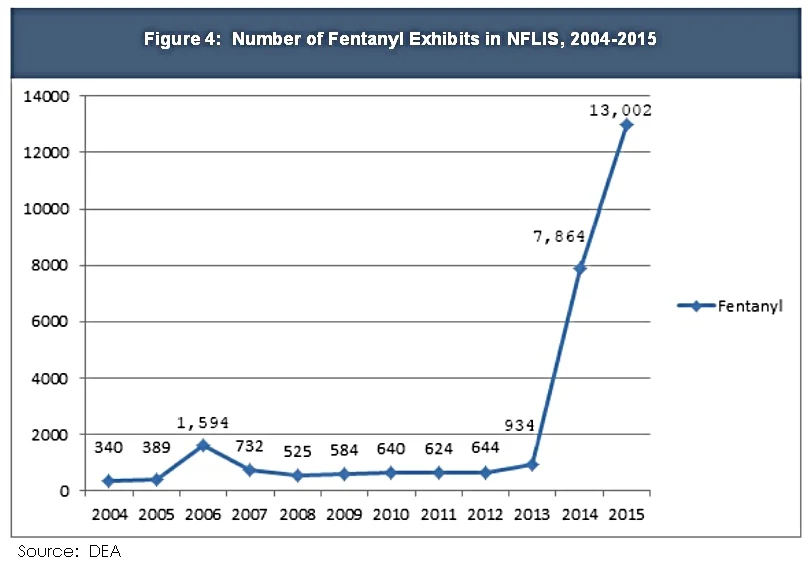
The report highlighted the fact that U.S. forensic laboratories tested over 13,000 seized drugs containing fentanyl in 2015, up sharply from less than a thousand cases two years earlier.
The DEA said counterfeit pills are being smuggled into the U.S. from Mexico and Canada. Traffickers usually purchase powdered fentanyl and pill presses from China, and pill press operations have recently been found in Los Angeles and New York.
The counterfeit drugs problem is so serious the DEA believes it is undermining efforts to limit opioid prescribing.
“The arrival of large amounts of counterfeit prescription drugs containing fentanyls on the market threatens to devalue such initiatives and replaces opioid medications taken off of the street,” the DEA said. “Although not all controlled prescription drug users eventually switch to heroin, fentanyl-laced pills give DTOs (drug trafficking organizations) broader access to the large controlled prescription drug user population, which is reliant upon diversion of legitimate pills. This could undermine positive results from the state Prescription Drug Monitoring Programs, as well as from legislative and law enforcement programs.”
As Pain News Network has reported, Massachusetts and Rhode Island recently said fentanyl was to blame for nearly 60 percent of their opioid overdose deaths.
Senators Urge DEA to Reduce Supply of Opioids
A group of U.S. Senators is urging the DEA to "aggressively combat the opioid epidemic," not by going after fentanyl traffickers, but by making legal opioids even harder to get.
In a letter to acting DEA administrator Chuck Rosenberg, Senators Dick Durbin (D-IL) Sherrod Brown (D-OH), Edward Markey (D-MA), Amy Klobuchar (D-MN), Angus King (I-ME), and Joe Manchin (D-WV) urged the agency to tighten its annual quotas for manufacturers to produce controlled substances.
"In effect, DEA serves as a gatekeeper for how many opioids are allowed to be legally sold every year in the United States. Yet, for the past two decades, DEA has approved significant increases in the aggregate volume of opioids allowed to be produced for sale," the letter states.
The Senators urged the agency to rollback a 25 percent increase in production quotas for Schedule II opioids that was implemented in 2013. Schedule II opioids include hydrocodone, a widely prescribed painkiller that was reclassified from a Schedule III to a Schedule II drug in 2014.
The Senators also said the DEA should make a mid-year adjustment in the quota to immediately reduce the supply of prescription opioids. The letter did not address the fentanyl crisis or the rapid growth in counterfeit medication.