It's Time for Chronic Pain Patients to Act
/By Alessio Ventura, Guest Columnist
I am a chronic pain sufferer who recently had multiple emergency surgeries due to sepsis infection after a shoulder replacement.
I have had 17 surgeries since 2008, including major back surgery, rotator cuff repair, biceps tendonitis, knee surgery and hernia surgery. Bottom line: my body is now wracked with arthritis and post-surgical pain.
I have tried several pain treatment modalities over the years, including Lyrica, Cymbalta, chiropractic, injections, NSAIDs, and acupuncture. The only effective treatment in my case has been the legitimate, professional application of opioid medicine by pain management physicians.
I have severe allergic reactions to NSAIDs, which kill 15,000 per year and send 100,000 to the hospital. A friend of mine died from a stroke because of NSAIDs.
After my recent surgeries related to the shoulder replacement and subsequent infection, my wife had to travel to 25 different pharmacies before she finally found someone willing to fill my scripts for Oxycontin and Percocet.
This is not unusual though. Each month is a long trek to find pain medicine. What has happened due to government restrictions on opioids is a reduction in the supply of opioid medicine. The drug companies see the writing on the wall and are slowly trying to get out of the business.
ALESSIO VENTURA
At the same time, the government sets limits on how much a pharmacy can stock. That is according to pharmacists I have spoken to, but is denied by the DEA and FDA in response to letters I have written.
It truly is a nightmare. Each month, you have to go to pharmacy after pharmacy before you find a pharmacist willing to dispense the medicine, which pharmacists are under no legal obligation to provide. Many pain patients go into withdrawal each month as they search, while at the same time enduring intractable pain.
Most of us have tried every single alternative to opioids, but the anti-opioid hysteria paints a picture that there are better and safer therapies. That simply is not true. The only thing that works for many of us is an opioid-based medicine.
The madness is spreading. New Jersey governor Chris Christie has signed into law a bill that limits the first script for opioids to 5 days. After the four surgeries I’ve had since August, I was bedridden and could not visit a doctor after 5 days. They could not identify the infectious agent as they were unable to grow it in cultures. Eventually I was treated with 3 broad spectrum antibiotics, which in addition to killing the infection, also killed the "good" bacteria in my system, which caused severe fatigue and gastrointestinal side effects.
Many acute traumas, like when someone is shot or in a horrible car accident, will not provide for easy travel to visit a doctor to refill an opioid after 5 days, and it is currently illegal for a doctor to call in a script for controlled substances. This caused a run on opioid medicine in New Jersey as hospitals and surgery centers accumulated as much as they could, and with the cutback by drug companies, many people could not get their scripts filled.
My 85 year old mother in New Jersey had back surgery recently. My sister drove to 30 pharmacies -- starting in Bridgewater and working her way along Route 22 toward Newark -- and she was unable to get our mother’s scripts filled. My mother was in horrible pain and my sister had to rush her back to the ER. It was horrible. My sister broke down in tears at the ER as she explained her plight and the suffering of my mother.
There is a reason why army medics carry morphine to the battlefield. It is the only thing that has a chance to address severe acute pain.
In addition to supply limits, there is the prescription drug monitoring system. The government now tracks every single opioid that you legally acquire. If for whatever reason you find yourself away from home and cannot see your physician and you attempt to refill or get new pain medicine because of an injury, surgery or chronic pain, you will not be able to do it legally without first getting in touch with your doctor so they can coordinate care. Often this is not possible.
If you do get pain medicine while away without coordinating, you will be investigated and may be subject to arrest. Your doctor may also drop you from their practice. Your rights as a patient, especially your privacy rights and your right to seek pain relief, are now severely trampled.
Politicians are playing with fire as the opioid hysteria grows. More people will commit suicide rather than live with intractable pain, because politicians think they know more than doctors treating patients.
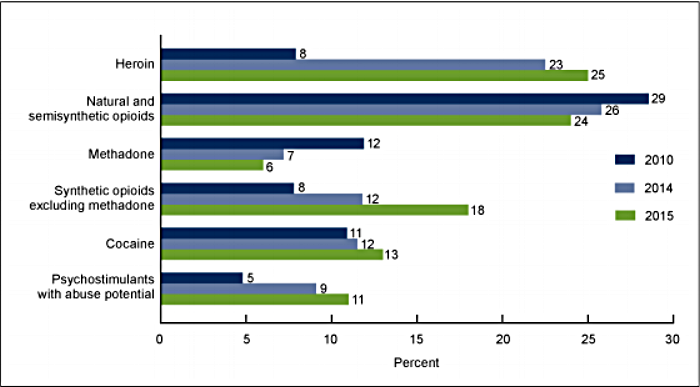
Who is going to listen to us? Politicians and some in the medical community conveniently conflate overdose data from the illegal use of opioids with legitimate use for intractable pain. They are also dismissive and try to tell us that we should try alternatives. For example, Lyrica is now being pushed by many, but it was developed only for a specific class of nerve pain, and possible side effects include suicide, weight gain, and a host of other things.
I almost committed suicide myself after being prescribed Lyrica and Cymbalta. I went from 190 pounds to 300 pounds, and had suicidal thoughts almost from the outset. When I told my doctors, they said, "Give it more time, the side effects will subside".
After the Lyrica and Cymbalta were stopped, I stayed on OxyContin and had bi-weekly testosterone shots. I lost all of the weight and the suicidal thoughts went away. It was a miracle.
There is a literal civil war occurring now between physicians who understand pain, and others who refuse to admit the truth about the efficacy of legitimate pain management via the use of opioids. Unless we all collectively speak up and scream loudly, meaning writing formal, respectful, but firm and forceful letters to our representatives, they will continue to step on us and cause our lives to be living hell.
It is time. Find out who your state and federal representatives are. Find out who your local, state, and federal health organization leaders are. Write formal letters, not emails or phone calls, to your representatives. After you write your letters, request meetings with your representatives and go to that meeting. Do whatever you can in a professional, respectful, but aggressive way in order to bring attention to our plight.
The time is now. Failure to act most assuredly means an end to our rights, a lifetime of pain, more illegal use of drugs, and in many cases, death.
Alessio Ventura was born in Italy, came to the U.S. at 17, and finished high school in Newark, New Jersey. He worked for Bell Laboratories for 35 years as a network and software engineer. Alessio has been married for 35 years and has 4 adult children, including triplets.
Pain News Network invites other readers to share their stories with us. Send them to: editor@PainNewsNetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.