Surviving the Hurricane of Chronic Pain
/By Crystal Lindell, Columnist
I have recently started feeling better these last few months — a string of good days, I like to say — and it’s given me a chance to catch my breath and reflect on some of the crap I’ve endured over the last couple years.
For me, waking up one day with stabbing rib pain was like swimming along the river of life, only to be picked up by a hurricane, hurled back about 100 miles, and left to fight the raging current in water that was barely above freezing.
And yeah, it made about as much as sense as a hurricane in a river.
It was like everything I had accomplished had been taken from me, and instead of swimming forward, or swimming at all, I was literally gasping for air, about to drown every single day.
And people would come along and say, “Oh, I’ll pray for you!” And I’d be like, “Umm, I’m literally drowning! And there’s a hurricane! In a river! HELP ME!”
And they would say, “Well, if you really want to survive, you’ll give up gluten.” And I’d be like, “Umm, I just need a life raft! Giving up gluten isn’t going to help me!”
And they would say, “Well, if you were a horse, we would have let you drown by now.” And then they would laugh. And I’d be in the river, trying to survive the winds and waves and the rain.
And then someone with the best of intentions would come up to me and say, “Well, everything happens for a reason. I’m sure there’s some larger reason why you’re drowning.” And then they would walk away. On the land.
I spent almost six months on the verge of drowning. And eventually I just got so tired that I wanted nothing more than to close my eyes, fall back into the water, and let it all go. Let the pain go. Let the depression go. Let the daily battle to stay above water, go.
I spent every day wanting to let go. Planning ways to let go. Convincing myself that if my family really loved me, they would just let me go.
I also started stripping away everything I could so that I could stay above water. I got rid of my part-time job as a church youth leader. I threw my independence over board and moved in with my mom. And eventually, heartbreakingly, I even let go of my boyfriend’s hand. I let it all slip away so I could focus all of my energy, every day, on breathing in air instead of filling my lungs with water.
And I tried to see every doctor I could find, looking for a lifeguard. But they would say things like, “Well, you don’t look like you’re drowning.” Or, “Well, I mean, you’re drowning. But we can’t see the hurricane, so there’s not really anything we can do about it.”
And then, finally, a rescuer came along. We will call him, Dr. M, for Miracle. I literally tear up when I think about meeting Dr. M.
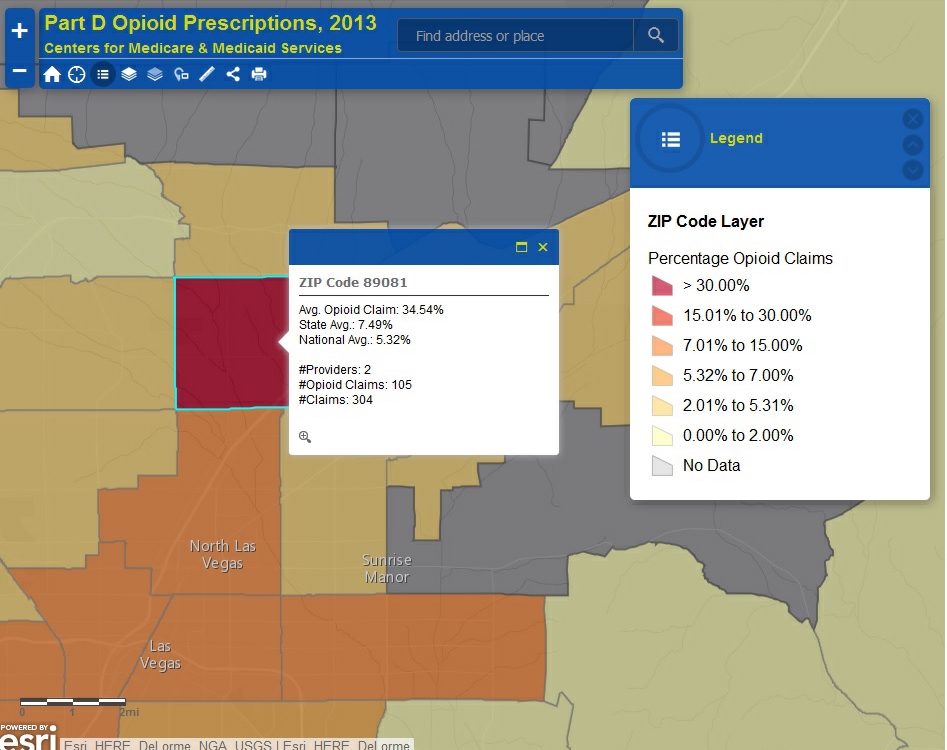
He couldn’t see the hurricane either, but he believed me when I said there was one. And he understood the one thing I needed more than anything was a life raft. So he threw me one. Dr. M put me on a large dose of opioids, and it was the best thing that could have ever happened to me. It was like someone calmed the winds and the storm started dying down. The water finally got still for the first time in a long time.
He was the first doctor to actually take my pain seriously. I imagine that he’s either had chronic pain himself, or loves someone who had it because that’s the only way I can explain how compassionate he was — how amazing he was about believing that I was truly drowning.
It’s true that the best thing you can say to someone who is sick is, “I believe you.”
It was because of Dr. M that I finally got on a drug regimen that allowed me to float in the water every once in a while and rest my arms. To let the life raft do some of the work. And when I told him that the medication wasn’t lasting me all month — that, near the end of the 30 days, I was starting to drown again — he believed me, and gave me enough to get through all four weeks.
But even with the drugs, the only thing I could really do was float. I couldn’t swim forward or even get to shore. I just stayed still, trying to survive all the times the winds picked up, or the water got below freezing, or the waves got too big. I did my best to endure the side effects from the medication, the pain flares, and the ER visits.
There’s a saying, “You’ve got what it takes, but it will take everything you’ve got.” And surviving this has taken everything I ever had in my soul.
For the last two years though, I’ve just been happy to still be alive. Happy that I had a life raft and some calmer waters. I started planning how to live my life where I was. It was 100 miles behind where I’d been, but I started to realize that the trees in that area were actually kind of pretty. And that there were some other people floating around that I would have never met if there had never been a hurricane. I started to think that perhaps I could set up a life there.
But then, something happened. Something I never thought would ever happen, actually happened. I started swimming forward again.
I had tried every day that I could to swim forward, only to be pushed back. I would wake up and try to shower, go for a walk, drive, or do anything that would help me go forward again. But every time, I ended being tossed right back to where I was — sometimes even further back.
One day though, I swam forward and I stayed there. And then the next day, I swam forward a little more, and I stayed there too. And then again, again and again.
I had started taking vitamin D, after realizing that I was tragically deficient in what should more accurately be referred to as hormone D. When I started getting my levels back up it was like I suddenly had the strength to move forward again. My whole body could swim again.
And for the first time in a long time, I experienced things I had almost forgotten existed. The perfect pleasure of going for a long walk on a crisp fall day. The heart-stopping independence of being able to get in car, drive myself to the mall, and do the one thing I used to love most of all — shop. The joy of being able to take a shower and immediately blow dry my hair without needing an hour-long break in between the two.
There were so many things that I couldn’t do because I couldn’t swim forward for so long. So many things I had to give up. Like folding my own towels in my own special way. And waking up to the sunrise and being happy to see the morning light without having to worry about the pull of fatigue from my medications.
And even, especially, turning over and laying on my right side. I had not laid on my right side in over two years.
So now, here I am, finally swimming forward again for the first time in a long time. For now, it feels like maybe the hurricane has finally passed. But I still wake up every day worried that there will be another storm. I worry that the winds will pick up and I’ll be hurled backward, and I won’t have a life raft and I’ll start to drown again.
But now, at least, I know that if that does happen, I have it in me to survive.
Crystal Lindell is a journalist who lives in Illinois. She loves Taco Bell, watching "Burn Notice" episodes on Netflix and Snicker's Bites. She has had intercostal neuralgia since February 2013.
Crystal writes about it on her blog, “The Only Certainty is Bad Grammar.”
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represent the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.