Why Are They Being So Cruel?
/By Debbie Duke, Guest Columnist
I am 63 years old and have been on pain meds consistently since the age of 38. I have systemic lupus and scleroderma, which fortunately is in remission. I also suffer from gout, fibromuscular dysplasia, scoliosis, kidney pain and post-operative pain from breast cancer surgery.
My experience with pain management doctors in the beginning was very pleasant and I was getting relief from my agony. I was disabled but still functional due to pain medication.
But recently things have changed. After several years of using a pain pump, I decided to go back to oral medication to have more control. The pump was not that effective for breakthrough pain and made me feel disconnected. After giving up on the pump, I changed doctors and the new one gave me the medication I had been before.
On my last visit, he said a new law requires patients on pain meds to have no more than the equivalency of 90mg of morphine. Then he cut my dose in half. I am now in agony and can see why people would turn to other ways of getting relief or decide to end it all.
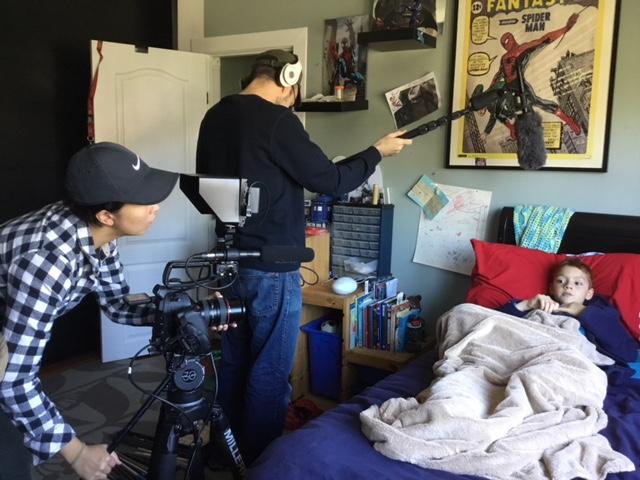
I love life and have many reasons to live. I care for a grandchild who had nearly been lost to foster care. Now, due to my inability to get around very well, I may not be able to continue taking care of her.
DEBBIE DUKE
I can't bear to think of it.
Why are they being so cruel to those of us who are law abiding, while the crooks get away with it? When someone grabs grandma's meds from her purse or medicine cabinet, why is that grandma’s fault?
Overdoses have been around for years and years. Who did we blame? The one who stuck the needle in their arm, that's who. Yes, we have a drug epidemic, but do something about the drugs coming across our borders. There has been enough squeezing of patients. Give them what works for them. It sickens me to see patients treated unjustly turning to other ways to help themselves.
I'm truly afraid that everything in my life as I know it will end. Thanks to irrational politicians who have taken away our right to be as free of pain as possible.
I think sometimes about what will be said in the future. We'll be saying, “Remember the days when we were able to have pain relief and no one had to suffer?”
I know that people are dying, but to equate prescriptions with illegal drugs to make some political point is wrong. I wish those that are in pain could march down Pennsylvania Avenue. But we are too sick for that.
Debbie Duke lives in Florida.
Pain News Network invites other readers to share their stories with us. Send them to editor@painnewsnetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.