Pennsylvania Overdoses Soar, But Not from Painkillers
/By Pat Anson, Editor
A new study by the U.S. Drug Enforcement Agency underscores the changing nature of the nation’s overdose crisis and the diminishing role played by opioid painkillers.
In an analysis of 4,642 drug related overdose deaths in Pennsylvania last year, the DEA found that over half of those deaths (52%) involved fentanyl or fentanyl related substances. In many cases, toxicology reports found multiple drugs in the bodies of those who died.
Heroin was the second most frequently identified drug (45%), followed by benzodiazepines (33%), a class of anti-anxiety medication, and cocaine (27%).
Prescription opioid medication was the fifth most common type of drug found. Painkillers were involved in 25 percent of the Pennsylvania overdoses, while ethanol (alcohol) was ranked 6th at nearly 20 percent.
Overall, the number of overdoses in the state was 37 percent higher than in 2015, according to the DEA report. Pennsylvania's overdose rate was 36.5 deaths per 100,000 people, twice the national average.
Fentanyl is a synthetic opioid 50 to 100 times more potent than morphine, and is available legally by prescription to treat severe chronic pain. In recent years however, illicit fentanyl has become a deadly scourge across the U.S. and Canada, where it is often mixed with heroin or used in counterfeit painkillers. Illicit fentanyl is believed to be involved in the vast majority of the fentanyl-related deaths in Pennsylvania.
DRUGS INVOLVED IN PENNSYLVANIA OVERDOSES (2016)
The DEA report was prepared in conjunction with the University of Pittsburgh’s School of Pharmacy Program Evaluation Research Unit (PERU). Unlike other reports on overdose deaths, the PERU analysis excluded suicides and included toxicology reports, a methodology that is considered more reliable than the ICD codes traditionally used by the CDC and other federal agencies to determine the drugs involved in overdoses.
“The expertise of PERU in the analysis and interpretation of public health data, which is outside of the traditional scope of law enforcement intelligence analysis, resulted in the creation of this comprehensive report that can be used to implement effective strategies to address the overdose crisis,” said Gary Tuggle, Special Agent-in-Charge of DEA’s Philadelphia Field Division.
Perhaps the most striking aspect of the report was the presence of anti-anxiety drugs in so many of the overdoses, and the smaller role played by prescription opioids. Toxicology reports found opioid medication in 1,181 of the overdose deaths, with oxycodone involved in most of them.
Still, more Pennsylvanians died with Xanax (alprazolam) in their system than oxycodone (846 vs. 679). And the anti-anxiety drugs clonazepam (Klonopin), diazepam (Valium), oxazepam and lorazepam (Ativan) were also involved in hundreds of overdoses.
The existence of valid prescriptions was not analyzed in the DEA report, which did not assess whether medications were diverted or obtained fraudulently.
In 2016, approximately 13 people died of a drug-related overdose in Pennsylvania each day.
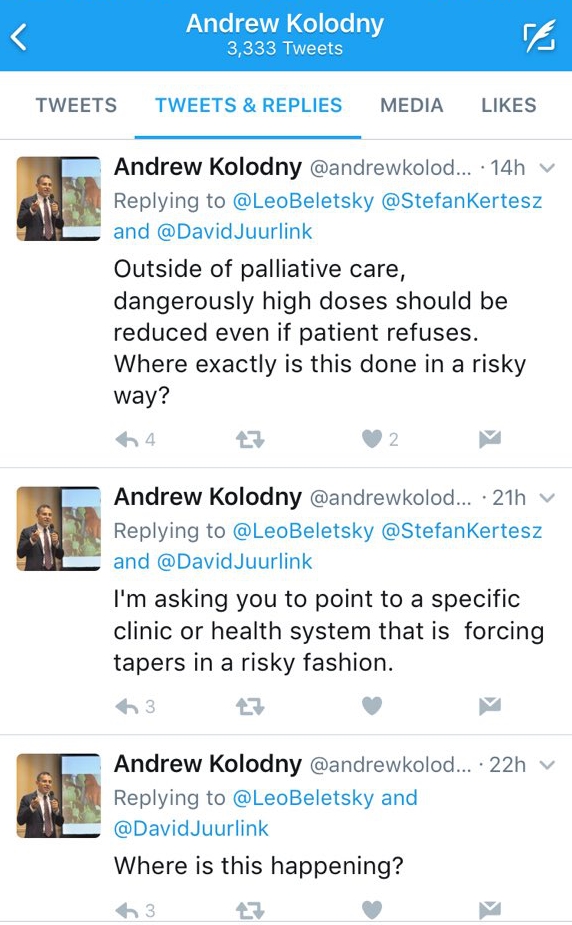
Although painkillers were not involved in most of those deaths, efforts at fighting the overdose crisis are still largely focused on reducing access to legally prescribed opioid medication.
Last month, Independence Blue Cross, the largest health insurer in the Philadelphia area, said it would limit the prescribing of opioids in its network to just five days for acute pain. Independence already limits the quantity of opioids that physicians can prescribe. The company claims that policy has reduced "inappropriate" opioid use by its members by nearly 30 percent.
Deaths from prescription opioids in Philadelphia started declining in 2013, a year before Independence started limiting access to painkillers.