The PAIN GAME: How Pain Medicine Was Criminalized
/By Dr. Lynn Webster
“What happened?”
It’s the most basic question you can ask about the opioid crisis. Yet for more than two decades, most of the answers the public has been given have been pre-packaged: Greedy drug companies, corrupt “pill mill” doctors, desperate patients, and a heroic legal system swooping in to clean up the mess.
What almost no one has seen is what was happening inside those prosecutions as they unfolded; in the homes of the accused physicians, in the war rooms of their defense teams, in the quiet panic of the patients who depended on their care.
That’s what makes The PAIN GAME so extraordinary.
More than twenty years ago, filmmaker Erica Modugno Dagher did something journalists almost never do: she embedded herself at the center of an unfolding legal, medical, and political firestorm and started asking, with a genuinely open mind, “What happened?”
Then she kept the camera rolling for two decades.
Writer and editor Amy Bianco, who now authors The PAIN GAME on Substack, has taken that trove of footage, documents and human stories, and begun unpacking how the legal system — especially the DEA and federal prosecutors — systematically confused pain medicine with crime, and how that confusion still harms patients today.
If you want to understand why doctors are afraid to treat pain, and why patients are still paying the price, I’d urge you to start with Bianco’s first episode. It’s one of the most important stories you’ve never heard.
Targeting Doctors
The origin of The PAIN GAME runs through the work of political scientist Ronald Libby, PhD, whose 2007 book “The Criminalization of Medicine: America’s War on Doctors” documented a wave of prosecutions in which physicians were recast as criminals.
Instead of tackling the hard work of healthcare reform or rational drug policy, federal and state authorities went after doctors who billed heavily to Medicare and Medicaid, especially those caring for poor and disabled patients with complex pain.
According to Libby, the logic was simple and brutal:
High billing = “fraud and abuse”
High opioid prescribing = “drug dealing”
Under that lens, the DEA and U.S. attorneys didn’t need to understand the nuances of chronic pain, palliative care, or Ehlers–Danlos syndrome. They just needed numbers: prescription counts, morphine milligram equivalents, and outlier billing profiles.
The more a physician’s practice reflected the grim reality of caring for very sick people, the more suspicious they looked on a spreadsheet.
By the early 2000s, news outlets were saturated with stories of “pill mills” flooding communities with OxyContin. Those stories had a ready-made villain and an easy fix: prosecute the doctor, shut down the clinic, and declare victory.
But as The PAIN GAME shows from the inside, it didn’t add up.
A Camera Inside the Crackdown
Because Libby had earned the trust of embattled clinicians, that trust extended to Erica. She was invited into defendants’ homes, their lawyers’ strategy sessions, back-hall conversations at medical and legal conferences, and even the corridors of Congress.
Crucially, she went in without an agenda. There was no narrative she needed to confirm and no “pill mill” caricature she had to deliver. She simply watched and listened as doctors, patients, lawyers, and advocates tried to understand why the government had suddenly turned medicine into a crime scene. That is what makes the series riveting.
Amy’s first episode on Substack tells this origin story from the inside. She weaves in her own path through the pain world, including her friendship with chronic pain advocate Siobhan Reynolds, founder of the Pain Relief Network, and her own diagnosis with Ehlers–Danlos syndrome. She then patiently walks readers through what the footage and documents reveal.
What emerges is not a defense of every prescribing decision ever made. It is something more unsettling: a portrait of a legal system that decided it was easier to dramatize a few high-profile prosecutions than to grapple with the real drivers of overdose and despair.
When the DEA Writes Medical Policy
Once you see these cases from the inside, the larger pattern comes into focus.
Prosecutors leaned on cooperating witnesses, often people who themselves had been charged, to transform complex medical practices into simple crime stories.
DEA agents and auditors treated prescribing volume as guilt, with almost no capacity to distinguish a high-complexity referral practice from a storefront drug operation.
The media, fed a steady diet of press releases and perp walks, amplified the “drug dealers in white coats” narrative until it hardened into common sense.
And while those courtroom dramas played out, something quieter, and more damaging. was happening across the country.
Doctors who were never criminally charged saw colleagues indicted or their offices raided — which led them to decide that continuing to treat high-risk patients simply wasn’t worth taking the chance.
Pharmacists also grew skittish about filling legitimate prescriptions. Medical boards and hospital systems imposed rigid rules, less in the service of good medicine than to signal compliance and to distance themselves from the crisis that had been miscast in the public eye.
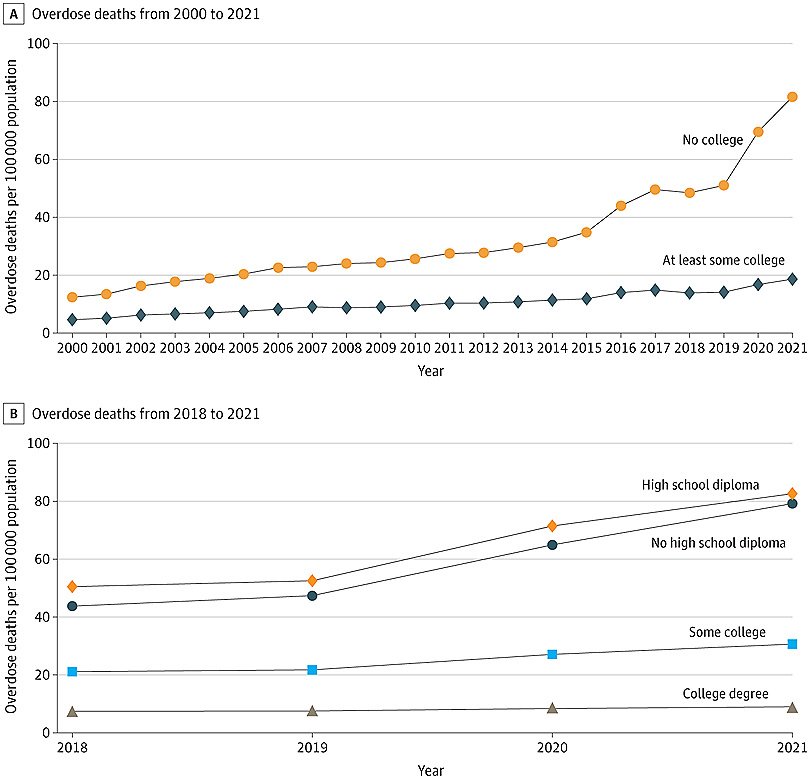
The overdose crisis surged forward in the meantime, driven increasingly by illicit fentanyl and a volatile street supply that no prosecution could touch. Prescribing plummeted, while overdose deaths soared.
This is the great irony The PAIN GAME helps expose: The very tools we were told would “fix” the crisis — aggressive DEA enforcement against prescribers — did little to curb overdoses. But they have been devastatingly effective at making it harder for people in pain to get care.
Why The Pain Game is Timely Today
You cannot reconstruct this history by looking backward. Many of the key players are gone. The media environment has only grown more hostile toward anyone who challenges the standard narrative about opioids. The raw fear that Libby detected in the early 2000s has turned into a kind of enforced silence.
That’s why Bianco’s work on The PAIN GAME is so valuable. She and Erica were there as it happened. I have learned that they turned over every page in their research: trial transcripts, medical records, internal memos, and obscure legal filings. They followed the story from exam rooms and courtrooms all the way to Capitol Hill, and they never stopped asking, “What actually happened here?”
If you care about pain medicine, civil liberties, or the rule of law, you’ll find The PAIN GAME both captivating and deeply sobering. It shows, in human terms, how we let a criminal justice narrative substitute for real health policy, and how that mistake still shapes the lives of patients and clinicians today.
The first episode is your entry point into that world. Read it. Sit with it. And then, if you find yourself thinking, No one ever told this part of the story, hit the subscribe button on Amy Bianco’s Substack.
We cannot undo the damage that has been done, but we can tell the truth about how it happened. The PAIN GAME is one of the few places where that truth is being documented, carefully and courageously, in real time.
Lynn R. Webster, MD, is a pain and addiction medicine specialist and serves as Executive Vice President of Scientific Affairs at Dr. Vince Clinical Research, where he consults with pharmaceutical companies.
Dr. Webster is the author of the forthcoming book, “Deconstructing Toxic Narratives -- Data, Disparities, and a New Path Forward in the Opioid Crisis,” to be published by Springer Nature.