PROP Ends Affiliation with Phoenix House
/By Pat Anson, Editor
Physicians for Responsible Opioid Prescribing (PROP), an influential and politically connected advocacy group that seeks to reduce opioid prescribing, is no longer directly affiliated with Phoenix House, which runs a nationwide chain of addiction treatment centers.
The Steve Rummler Hope Foundation is now the “fiscal sponsor” of PROP, which will allow PROP to collect tax deductible donations under the foundation’s 501 (c) (3) non-profit status. IRS regulations allow non-profits to form partnerships with like-minded organizations, allowing other groups to essentially piggyback off their non-profit status and collect donations.
Like PROP, the foundation’s main goal is to reduce opioid prescribing. It is named after Steve Rummler, a Minnesota pain patient who became addicted to opioid medication while being treated for a back injury.
After several attempts at addiction treatment, Rummler relapsed and died of a heroin overdose at the age of 43.
“He struggled with the pain for a long time,” said Judy Rummler, Steve’s mother and chief financial officer of the foundation. “He had what I think later was figured out to be some damage to the nervous system around his spinal cord because he had what he described as shooting electric shock-like sensations that would shoot up his back into his head and down his legs into his feet.”
Steve sought help from many doctors, but never received a treatable diagnosis. He started taking OxyContin for pain relief.
“Once he was prescribed the opioids in 2005, then he didn’t care about getting answers anymore,” his mother said.
After Steve’s death in 2011, the Rummler family established the foundation with the goal of helping others who also struggle with chronic pain and addiction. It was PROP’s founder and chief executive, Andrew Kolodny, MD, who approached the foundation with the idea of joining forces.
“Basically as the fiscal sponsor we accept donations and we manage the funding. We don’t set any policy for him,” Judy Rummler told Pain News Network. “Obviously our missions are similar. We are very concerned about the overprescribing of opioids. Yet I know if my son were alive today he would probably be telling you what you hear from so many other pain patients; that he couldn’t live without them. But the problem was he died as a result of it.
“I know there are a lot of people who are going to be hurt by cutting back on the prescribing, but I just think a lot of them are addicted as my son was. Yet he would have been the first one to scream and yell about having his pills cutoff.”
The Rummler Foundation calls this tug-of-war between opioids and addiction “The Dilemma.” It advocates for wholesale change in the treatment of chronic pain, emphasizing “wellness rather than drugs” and the use of “a wide array of non-opioid options.”
Opioid medication should not be prescribed for chronic pain, according to Rummler.
“I would never say that it’s impossible for it to work for someone. I wouldn’t say that. But I would say there’s no evidence it would work. And it shouldn’t be prescribed that way,” she said. “There are so many people dying. I hate to even use the term ‘abuse’ because I don’t think my son, really, I mean at the end he was an abuser, for sure. But it wasn’t abuse that got him addicted. It was the prescribing that got him addicted.”
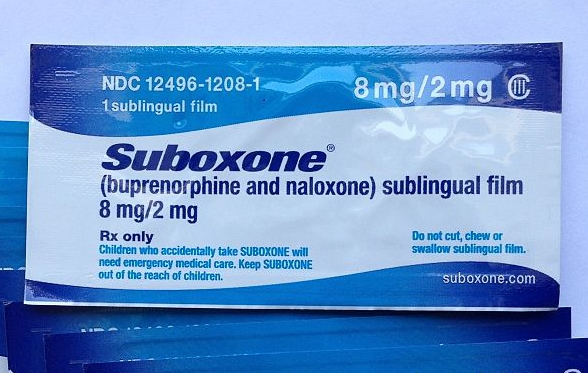
In addition to promoting awareness about opioid addiction, the Rummler Foundation sponsors prescriber education courses and provides free naloxone rescue kits to reverse the effects of opioid overdoses.
Links with PROP
The Rummler Foundation already has a lengthy association with PROP. Kolodny serves on the foundation’s medical advisory committee, as does Jane Ballantyne, MD, PROP’s president. The two groups have also participated together in several advocacy campaigns.
While PROP no longer considers itself “a program” of Phoenix House, Kolodny is still listed as the chief medical officer for the organization.
For several years, PROP lobbied the FDA, DEA and other federal agencies to reduce the prescribing of opioids with mixed success. Recently it played a significant role in the development of the CDC’s opioid guidelines, which discourage primary care physicians from prescribing opioids for chronic pain. Kolodny, Ballantyne and three other PROP officers and board members served on panels advising the CDC.
As Pain News Network has reported, Ballantyne and two other PROP board members are currently participating in CDC funded webinars to teach prescribers how to implement the guidelines. Those guidelines, which were released in March, have already had a significant impact on the pain community. In a recent survey, over two-thirds of patients said their opioid medication has been reduced or stopped by their doctor. About half said they have considered suicide as a way to end their pain since the guidelines were released.
In addition to his new affiliation with the Rummler Foundation, Kolodny is working with the Los Angeles-based Media Policy Center in developing a documentary on opioids and addiction. PROP is listed as one of the partners in the project, along with the Semel Institute of Neurobiology and the Geffen School of Medicine at UCLA.
The Media Policy Center (MPC), which declined to comment for this story, states on its website that it hopes to release the documentary in November and eventually air it on PBS.
“The best way to prevent deaths and overdose is through education,” MPC says in a statement on its GoFundMe campaign. “Many people have the misconception that opioids, such as OxyContin, are safe because they are prescription drugs, however, they are very addictive and once people lose access to their prescriptions or can no longer afford the drug they may turn to drugs like heroin.”
PNN has learned that several prominent doctors in the field of pain management have been approached to participate in a “debate” with Kolodny for the program. All have declined because they fear the documentary will be biased.