By Pat Anson, PNN Editor
Tomorrow the U.S. Drug Enforcement Administration holds another Prescription Drug Take Back Day, a campaign that encourages people to help combat drug addiction and overdoses by disposing of their unneeded medication at thousands of drop-off locations nationwide.
It’s also a day the DEA uses to further stigmatize the prescription drugs that millions of Americans rely on to control their pain and have functional lives.
“The majority of opioid addictions in America start with prescription pills found in medicine cabinets at home. What’s worse, criminal drug networks are exploiting the opioid crisis by making and falsely marketing deadly, fake pills as legitimate prescriptions, which are now flooding U.S. communities,” DEA Administrator Anne Milgram said in a statement. “I urge Americans to do their part to prevent prescription pill misuse: simply take your unneeded medications to a local collection site.”
The DEA’s campaign to reduce the supply of opioid medication goes well beyond drug take back days. In 2022, the agency is planning to cut production quotas for oxycodone, hydrocodone and other widely used opioid pain relievers. If the proposed quotas published this week in the Federal Register are adopted – and past history indicates they will be – it’ll be the sixth consecutive year the DEA has reduced the supply of opioid medication.
During that period, production quotas have fallen by 63% for oxycodone and 69% for hydrocodone. And opioid prescribing has fallen to levels not seen in 20-years.
But with drug overdoses climbing to record highs, critics say there is no evidence the DEA’s strategy is working. And they are alarmed that a law enforcement agency is setting policies that affect the healthcare choices of Americans -- in effect, practicing medicine without a license.
“I think a very strong argument can be made that DEA is inappropriately exercising medical judgment based on their reasoning for supporting another production reduction for opioid analgesics,” says Dr. Chad Kollas, a palliative care specialist in Florida. “Federal policy has encouraged blind reductions in opioid prescribing, so for DEA to cite that trend as evidence for a reduced need for the medical supply of opioid analgesics is a self-fulfilling prophecy.
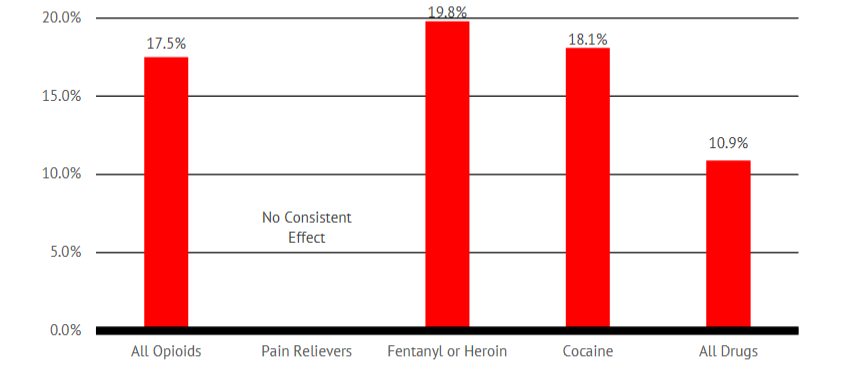
“Reduced prescribing has not led to a reduction in overdose deaths involving opioids, but rather has been associated with an increase in overdose deaths and suicides in patients with chronic pain who have been forced off their pain medications. Federal opioid policy calling for non-focused, reduced opioid prescribing has been an abject failure.”
18.88% Decline in ‘Medical Need’
Under federal law, the DEA is required to annually set production quotas for opioids and other controlled substances. It does so after consulting with the Food and Drug Administration, Centers for Disease Control and Prevention, and other federal agencies to establish the amount of drugs needed for medical, industrial and scientific purposes.
"The responsibility to provide these estimates of legitimate medical needs resides with FDA. FDA provides DEA with its predicted estimates of medical usage for selected controlled substances based on information available to them at a specific point in time in order to meet statutory requirements,” DEA explained in the Federal Register.
“With regard to medical usage of schedule II opioids, FDA predicts levels of medical need for the United States will decline on average 18.88 percent between calendar years 2021 and 2022. These declines are expected to occur across a variety of schedule II opioids including fentanyl, hydrocodone, hydromorphone, oxycodone, and oxymorphone."
Asked to comment on the DEA’s statement, an FDA spokesperson said the agency sent a letter to the DEA in April 2021 using pharmaceutical sales data from prior years to create “statistical forecasting models to estimate medical need for the next two years.” The FDA letter never actually used the 18.88% estimate, that was a figure apparently calculated by the DEA itself.
“In the letter FDA provided an estimate for need of each individual active ingredient in various opioid medications for 2021 and 2022. It appears the DEA estimated the 18.88% decrease as an average across the list of opioid active ingredients, presumably based on the estimates we provided. We do not disagree with their forecast for this decreasing trend of opioid need,” the FDA spokesperson wrote in an email to PNN.
Opioid ‘Red Flags’
In its statement in the Federal Register, DEA also said it relies extensively on data from prescription drug monitoring programs (PDMPs) to find “red flags” that may indicate a drug is being abused or diverted. The DEA is particularly concerned about daily opioid doses that exceed 240 morphine milligram equivalents (MME). That’s a very high dose for most people – and well above the CDC opioid guideline’s recommended limit of 90 MME.
“DEA believes that accounting for quantities in excess of 240 MME daily allows for consideration of oncology patients with legitimate medical needs for covered controlled substance prescriptions in excess of 90 MME daily. Higher dosages place individuals at higher risk of overdose and death. Numerous dispensings of prescriptions with dosages exceeding 240 MME daily may indicate diversion such as illegal distribution of controlled substances, or prescribing outside the usual course of professional practice,” the DEA said.
Where does the 240 MME threshold come from? That’s apparently another case of the DEA coming up with its own estimates to determine whether a dose is medical necessary. It certainly doesn’t come from the CDC guideline, which was never meant to include patients suffering from cancer pain or those in palliative care.
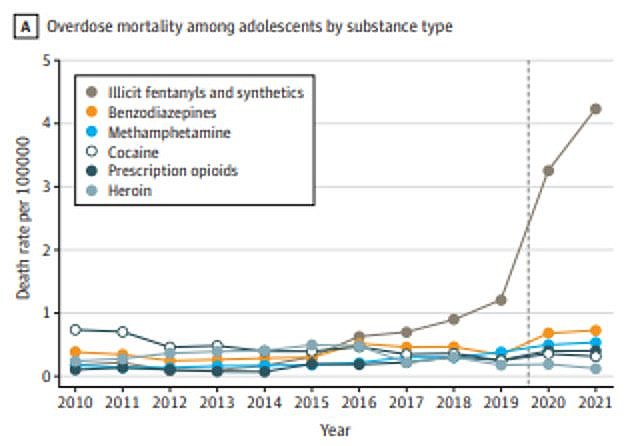
“The DEA is misapplying the CDC opioid guidelines, which were explicitly not meant to apply to patients receiving palliative care,” Dr. Kollas told PNN. “Moreover, it’s disingenuous for DEA to infer that patients receiving higher doses of opioid analgesics are diverting them, when the vast majority of opioid overdose deaths arise from illicit fentanyl in counterfeit pills.”
Just how serious is the drug diversion problem? Not so serious at all, according to the DEA’s own National Drug Threat Assessment, an annual report that for years has said that less than 1% of legally prescribed opioids are diverted.
“The number of opioid dosage units available on the retail market and opioid thefts and losses
reached their lowest levels in nine years,” the DEA’s 2020 report found.
The same report also found that illicit fentanyl, not prescriptions opioids, is “primarily responsible for fueling the ongoing opioid crisis.” That’s a view shared by the American Medical Association, which declared in 2020 that “the nation no longer has a prescription opioid-driven epidemic.”
‘Stop Punishing Pain Patients’
If that makes you wonder why the DEA is so intent on further reducing the supply of opioids, you’re not alone.
“This is pure insanity. The scientific data from the CDC & NIH (National Institutes of Health) show that the overdose crisis is NOT due to prescription opioid analgesics,” wrote Chuck Robertson, one of hundreds who left comments in the Federal Register on the DEA proposal. “We are in the midst of the worst supply chain crisis in modern history, so you want to continue to cut back on production? All this is doing is putting hospitals and pharmacies at risk of being short medications that people need to control pain.”
“Please don’t cut production quotas of the opioids listed. There are hundreds of stories of people who need opioid medication therapy to even live at the most basic of functionality,” said Michelle Stifle, a chronic pain patient for 22 years. “This inhumane treatment is discriminatory. Stop punishing pain patients for the faults of others.”
“Please do not cut the quotas anymore. My wife has several autoimmune diseases that cause horrible pain. She was completely cut off of her pain meds after almost 20 years of use,” said Jeffrey Smith. “She never took more than prescribed and never abused them. It allowed her to live somewhat normally. Now she suffers every day and has no life. I'm afraid the time is coming she won't be able to take the pain anymore.”
“I was forced tapered off my pain meds after taking them responsibly for 17 years. I now spend 75 percent of time in bed. I cannot function and am in constant pain,” said Shelly Allen. “I recently tore my rotator cuff and couldn't even get a few days’ worth. Where there may have been overprescribing there is now underprescribing. It's my body, why can't I choose my own pain relief in reasonable doses?”
“We don't need more cuts to the supply of opiates. It doesn't help avoid addiction or address it. All cutting the supply further will do is promote health care rationing,” wrote Amber Smith. “Opiates are necessary for surgery and other medical needs. Would the DEA ever suggest cutting the supply of chemotherapy or insulin? No, yet those are every bit as necessary to patients as opiates are.”
The DEA did not respond to a request for comment on this story. To leave your comment on the DEA’s proposed 2022 production quotas, click here. Public comments must be received by November 17.