Opioid Addiction Linked to Range of Health Problems
/By Pat Anson, Editor
An extensive new analysis of insurance claims has found that patients being treated for opioid addiction are much more likely to suffer from a wide range of other health problems, including hepatitis C, HIV, bronchitis, fibromyalgia and chronic pain.
The large study by Amino – a healthcare information company – looked at 205 million private health insurance claims involving patients with “opioid use disorder,” a loosely defined diagnosis that includes both mild and severe forms of “problematic” opioid use. The diagnosis does not distinguish between prescription opioids used therapeutically and illegal opioids such as heroin that are used recreationally.
In just four years, Amino found a 6-fold increase in the number of Americans diagnosed with opioid use disorder, from 241,000 in 2012 to 1.4 million 2016.
Amino also found that patients with opioid use disorder were significantly more likely to be diagnosed with diseases linked to substance abuse and intravenous drug use, including hepatitis C, HIV, alcoholism and mental health issues.
“Behavioral health issues like alcoholism and binge drinking were 8.4x and 5x more frequently diagnosed among patients who were also diagnosed with opioid use disorder, while mental health issues like suicidal ideation and post traumatic stress disorder were 6.9x and 4.2x more frequently diagnosed,” wrote Amino researcher Sohan Murthy.
Murthy and his colleagues also found many diagnoses related to pain, including chronic regional pain syndrome (CRPS), herniated disc, failed back syndrome, stenosis and fibromyalgia.
Stanford psychiatrist Anna Lembke, MD, a board member of Physicians for Responsible Opioid Prescribing (PROP), told Amino there is a high risk for addiction even when opioids are prescribed for a “bonafide” medical use.
“What I thought was really interesting was the correlation with failed back syndrome. Perhaps failed back syndrome is a risk factor for developing an opioid use disorder—and that could be part of the reason why this community experiences such chronicity and lack of improvement. This is a subgroup that’s especially vulnerable to opioid misuse,” Lembke said.
"Failed back syndrome" is a diagnosis used to describe patients who do not respond or whose pain grows worse after spinal surgery, injections or other "interventional" procedures. Ironically, these same procedures are often promoted as "non-opioid" treatments for chronic back pain.
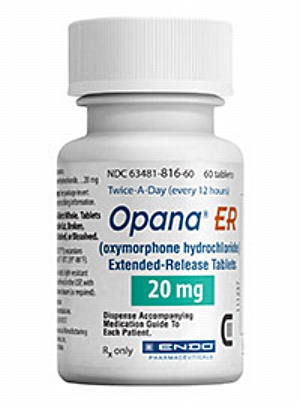
Amino notes in the study that the data does not make a "causal" link between different diagnoses, meaning the study doesn't conclude that opioid use disorder causes hepatitis C or HIV. However, the FDA recently asked that Opana ER be removed from the market because the painkiller was associated with outbreaks of hepatitis C, HIV and other diseases spread by intravenous drug use; indicating that health problems other than abuse and addiction are now being used by the agency as a rationale to limit the sale of opioids.
Amino found that geography is often a major factor in the diagnosis of opioid use disorder. The study found a disproportionate number of patients with opioid use disorder in Appalachia and Florida, suggesting that doctors in regions with a history of opioid abuse may simply be more likely to make the diagnosis. Kentucky alone had 9 of the top 10 counties for doctors treating a high volume of patients with opioid use disorder.