In 2018, senior analysts at the CDC revealed that for years, the number of overdose deaths the agency attributed to prescription opioids was vastly inflated due to problems with data collection classification. For example, deaths caused by illicit fentanyl were blamed on the prescription form of fentanyl, which is often used in emergency rooms.
Overdoses involving a combination of drugs were also misclassified. Last year, researchers concluded that, for over a decade, “millions of Americans” were “misled” by the CDC, politicians and the media to believe that the drug overdose crisis was driven by deaths caused by prescription opioids.
Patients prescribed opioids to treat long-term chronic pain are organizing across the country to overturn the CDC guidelines, and the debunking of CDC data and the AMA’s statement validated their cause. In interviews, multiple chronic pain patients said prescription opioids help them live more normal lives, but their lives became collateral damage of the war on opioid prescribing. Patients report that doctors refuse to treat them and pharmacies won’t fill their prescriptions, leaving them in disabling pain. Mothers are punished by hospitals after childbirth and even charged with crimes for continuing opioid therapy prescribed by a doctor during pregnancy.
“Opioids can be used safely during pregnancy, and we also know that when the response is immediately punitive or the application of the criminal legal system, there is actually far worse outcomes for babies and families, instead of being able to work that out with their doctor,” said Dana Sussman, deputy executive director of the National Advocates for Pregnant Women, in an interview.
Chronic pain patients and their advocates argue that the narrative linking opioid prescribing to the overdose epidemic is a “hoax,” and they are engaged in a pitched media battle with the “anti-opioid zealots” who pushed the CDC to discourage long-term opioid prescribing for anyone besides cancer patients and people dying in hospice.
Advocates point to research showing that rates of fatal drug overdose correlate with economic decline in many communities and have been rising rapidly since the late 1970s, not the mid-1990s when painkiller prescribing became more liberal thanks to campaigns by drug companies that have garnered plenty of headlines.
The prescribing debate is extremely emotional, with each side attacking the other over credentials and alleged ties to the pharmaceutical and biomedical industries. (Kertesz said he was attacked in the media by an “expert in the field” for simply announcing a study on deprescribing and suicides. “Attacking investigators in the absence of any knowledge of their work would not be customary behavior in any area of medicine,” he said in an email. “But in this topical area, it is.”)
“The way tapering is happening in the real world is just horrible, even for people who are using their medication appropriately,” Nicholson said.
‘Those Patients Went Through Hell’
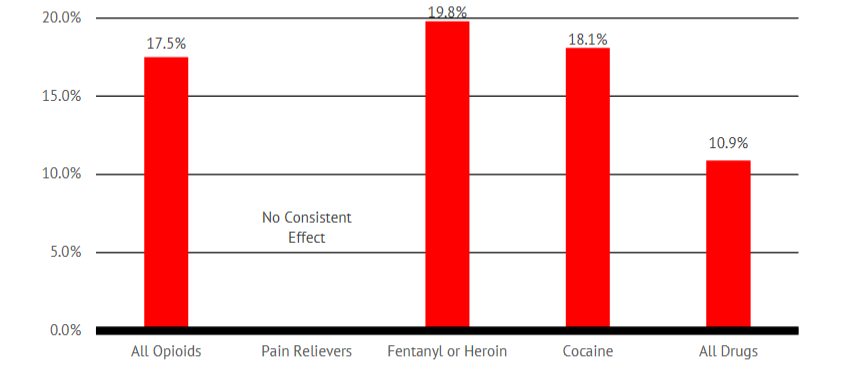
As an addiction specialist working at an emergency room and poison control center in Ohio, Ryan Marino has plenty of experience on the front lines. The narrative that overprescribing is causing an overdose crisis is clearly overblown, Marino said, because reductions in prescribing has not brought down deaths.
Marino says he often sees patients who were prescribed high doses of opioids for years until their medication was abruptly tapered or cut off after CDC prescribing “guidelines” became public policy and even law in some states.
“Those patients went through hell … naturally, some turned to street drugs because it is so miserable to have opioids cut off, whether you have addiction or not,” Marino told Truthout. “Seeing those patients has cast an additional shadow over this overdose epidemic that we are seeing, because the over-reactionary response is now creating additional harms.”
Marino said the manufacturing and dispensing of opioids can be a real money-maker in a for-profit health system, and overprescribing played a role early on in the crisis. At the same time, prescription drugs are much safer to use than illicit heroin and fentanyl. Marino said there are good arguments for access to a safe supply of opioids — including prescription heroin for people at high risk of overdose — because people using regulated opioids under medical supervision are far less likely to die.
“We need some sort of regulation [of prescribing], but the oversight the DEA provides seems more in line with reducing prescribing than ensuring that prescribing is appropriate and ensuring that people have access to prescriptions,” Marino said. “The reality is, most people who were using Oxycontin never wanted to switch to heroin, and people who were using heroin never wanted to switch to fentanyl.”
Kertesz, who has worked closely with low-income and houseless patients, also takes a nuanced view of prescribing. Like Marino, Kertesz said there were problems with overprescribing in the past, when medications were heaped upon patients instead of affording them more holistic care.
However, abruptly cutting patients off from medicines they depend on can cause all sorts of problems, particularly for people who have trouble consistently accessing health care in the first place. Doctors must make prescribing decisions based on the particular needs of a patient, but the crackdown has siloed prescribing as either “appropriate” or potentially illegal.
“We have now set up an entire system to push a change to care that does not have evidence for being safe or effective for patients,” Kertesz said.
For example, law enforcement often sees a “red flag” when patients are prescribed high doses of opioids or combinations of controlled substances, even when the prescriber is simply continuing the patient on a long-term regimen. While scrutinized by drug police as a sign of criminal activity, Nicholson said some patients benefit from drug combinations under appropriate medical supervision.
Kertesz said assuming something “criminal” is going on when patients are prescribed higher doses of opioids or more than one psychoactive drug at a time is “a big leap.” The same goes for other “red flags” drug police look for in statewide prescribing databases and records kept by pharmacies.
“A patient who has filled a script in two pharmacies, or a patient who has traveled a distance … anybody who has multiple complex needs is already suspect, anyone who is rural by definition is suspect,” Kertesz said. “Pharmacists are trying not to lose their jobs, so they transfer all this stigma and burden to patients.”
There is a difference between “drug dependence” and “drug addiction.” Addiction is characterized by impulsive drug use despite adverse consequences. Physiological drug dependence results from the continued use of many medications — not just opioids. Addiction is rare in patients prescribed opioids for pain, and while long-term use can create dependence, the benefits can also outweigh the harms. People living with opioid addiction may also be seeking relief from untreated pain, trauma or mental anguish.
Either way, abruptly cutting people off from opioids is dangerous. That’s why methadone and buprenorphine are prescribed for opioid addiction and dependence. Both drugs stabilize patients and stave off painful withdrawal symptoms, which is crucial for preventing overdose.
Advocates say the nuance is lost on the DEA and other law enforcement agencies. Drug cops are laser-focused on opioid “diversion,” the idea prescription opioids are being sold and used outside of their intended purpose. Data on diversion varies by source; a 2017 federal survey found that less than 11 percent of people who misused prescription opioids bought them on the street or stole them from a pharmacy or medical facility.
If the rest are “misusing” their own prescriptions or obtaining them from friends and family — an idea that often offends pain patients — then anti-diversion efforts are effectively targeting prescribers and patients themselves.
For years, the government and mainstream media claimed diversion was the source of the overdose crisis, even as the data began telling a much different story. There is plenty of anecdotal evidence, for example, that buprenorphine is usually diverted to people living with addiction. Vermont recently decriminalized possession of buprenorphine without a prescription for that reason.
The crackdown on diversion created grey areas that turned doctors and pharmacists into suspected drug dealers and patients into suspected criminals. In an ironic way, it worked. Pills became harder to find on the street, but reducing the supply did nothing to treat chronic pain or addiction. Overdoses involving illicit opioids are surging, and a growing chorus of drug users and advocates declare that “every overdose is a policy failure.”
The DEA did not respond to a list of questions by the time this article was published.
‘They Look at Prescribing as a Crime’
Joshi ran a general medical practice in Indiana, and he prescribed opioids for chronic pain as well as addiction. The DEA claimed Joshi was writing more prescriptions for controlled substances than most doctors in Indiana; Joshi says he served a population with serious medical needs.
It was the undercover DEA agent’s job to pose as a “drug seeking” patient and catch Joshi in the act of prescribing and secretly record it on video. Joshi says he tended to trust his patients, but trusting the undercover agent was his downfall. He also suspects a former employee wrote fraudulent prescriptions before becoming an informant for the DEA, although he has been unable to prove it.
“They are transplanting people in the health care field as a drug-dealing ring, so I am the captain drug dealer; you snitch on me and you go free,” Joshi said.
Terrified, Joshi accepted a plea deal after he was indicted on multiple drug charges. However, the DEA’s case against him shifted over time and relied on inconsistent witness testimony, leaving a federal judge frustrated when the time came for sentencing, according to a review of court documents.
The DEA accused Joshi of recklessly prescribing controlled substances, but prosecutors were unable to produce evidence that his patients did not have legitimate medical needs for the drugs Joshi prescribed. Multiple patients testified that Joshi’s practice made serious improvements in their lives. A day before Joshi was indicted, his clinic was recognized by the National Committee for Quality Assurance for “patient-centered, coordinated care.”
“A lot of people have it a lot worse than I do; there really wasn’t any evidence in my case,” Joshi said. “They essentially made a bunch of false statements.… Just the act of prescribing, it was construed as a crime. They don’t look at the clinical decision-making behind a prescription, they look at prescribing as a crime.”
A young doctor with a new practice and a child on the way, Joshi admits that he made mistakes. After losing his registration to prescribe controlled substances, Joshi says he unknowingly broke state rules by hiring nurse practitioners to write prescriptions for his patients. He also wrote a handful of prescriptions under another doctor’s name. Joshi says he tried to find workarounds out of concern for his patients. He did not want their “continuum of care” to be interrupted, but the judge saw a violation of the law.
“I tried to do what was right for my patients, but that was a deviation against the regulatory policies,” Joshi said.
Joshi was sentenced to 15 months in prison for writing an unnecessary prescription to an undercover DEA agent. He got out a few months early on good behavior. By the time he was sentenced, many of his patients were receiving the same treatment they had received from Joshi from other doctors.
Stephanie and Ashley were not so lucky. Both women overdosed and died after law enforcement suddenly interrupted their medical care and their safe supply of medication ran out.
*Ashley’s name has been changed to protect her identity.
This article is part of Truthout's series, "The Policing of Pain: Inside the Deadly War on Opioids."
Copyright © Truthout. Reprinted with permission.