Medicare May Stop Paying for Peripheral Nerve Blocks
/By Pat Anson
A public comment period will end soon on a proposal that could dramatically limit coverage of peripheral nerve blocks (PNB) and nerve ablation procedures for Medicare patients suffering from chronic nerve pain.
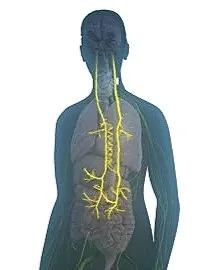
A PNB generally involves the injection of an anesthetic or corticosteroid into an injured area to block the transmission of pain signals. Under the proposal, all PNBs and nerve ablation procedures would no longer be covered for any pain condition, and the number of steroid injections and radiofrequency ablation procedures for nerve pain and trigeminal neuralgia would be limited.
Five Medicare administrative contractors (MACs) representing 24 states made the proposal in September and public comments will be accepted until November 22. MACs are private insurers that process Medicare claims and determine what coverage is “reasonable and necessary.”
In this case, they’ve determined that PNB’s and other nerve procedures have little or no benefit, and “therefore are not considered medically reasonable and necessary.” If approved, the proposal could be adopted by MACs in other states and become de facto Medicare policy nationwide.
Not surprisingly, there is opposition to the MAC proposal from healthcare providers who perform the procedures, who claim denial of coverage would force millions of chronic pain patients “to turn to opioids or less effective treatments.”
“For decades, chronic pain patients have received treatment from PNBs and ablation techniques that provide rapid and durable pain relief, enhance function and quality of life, and decrease reliance on systemic pain medications, including opioids,” said Patrick Giam, MD, President of the American Society of Anesthesiologists.
“We urge Medicare to consider the compelling clinical and functional evidence that supports coverage of PNBs and related procedures.”
“Unless the MACs want more Americans to be unable to work, reliant on opioids, and suffering in pain, it’s hard to understand their motivation here,” Tricia Pendergrast, MD, an anesthesiology resident at the University of Michigan, wrote in a recent STAT News op/ed
“Eliminating peripheral nerve block coverage will not result in meaningful cost savings from these patients, and may lead to more frequent emergency department and clinic visits, increased use of opioids and other pharmacologic interventions.”
As an alternative to injections and nerve blocks, the MAC proposal suggest the use of anti-depressants, gabapentin, topical lidocaine and transcutaneous electrical nerve stimulation (TENS) as first-line treatments for neuropathic pain.
Pregabalin, tramadol, capsaicin patches, Botox injections, and psychotherapy would be considered second-line treatments.
Opioids should only be considered as a third-line treatment, according to the MAC proposal, “as a last resort.”
Another effort to limit coverage of chronic pain treatments for Medicare patients begins in January. That is when Medicare is launching a 6-year pilot program in six states that will use artificial intelligence (AI) to review prior authorization claims for epidural steroid injections, cervical fusions, spinal cord stimulators, arthroscopic knee surgery, and other pain treatments.
Medicare considers the treatments to be “low value,” potentially unsafe, and ripe for fraud and wasteful spending.
The Wasteful and Inappropriate Service Reduction Model will cover Medicare patients in New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington who seek treatment for chronic pain, impotence, incontinence, and burns or wounds needing skin and tissue substitutes.