My Migraine Journey: From Electrodes to Cannabis
/By Gabriella Kelly-Davies, PNN Columnist
The room swirled as my eyes fluttered open, and I could feel something tight around my neck. It felt like a vice, making it difficult to swallow. The antiseptic smell was familiar, but I couldn’t quite place it. Struggling to focus my eyes, I heard a voice I knew well — it was Ben, a doctor at the hospital where I worked as a physiotherapist.
“How do you feel?” Ben said, shining a bright torch into my eyes.
“Where am I?”
“You’re in emergency. An ambulance brought you here. You were lying on the side of the road, unconscious.”
Ben told me the ambulance officers had received reports of cyclists being pushed off their bikes at the quieter end of the beach. They assumed that’s what had happened to me.
That day, my twenty-fourth birthday, heralded the onset of a life of migraine attacks.
Gabriella Kelly-Davies
During the 1990s, I regularly traveled around Australia for work while studying business at night. In the plane as I read my textbooks, a pain like an electric shock would shoot up the back of my neck and head.
It lasted for several minutes, then a deep ache started in the base of my skull. The pain eventually spread upwards, fanning out until it covered the entire back of my head and temples.
All too soon, the pain I experienced while flying became more regular and was most severe after sailing and playing my piano or cello. Cycling and tennis also triggered it.
In 1996, I started a job in Parliament House, Canberra as a policy adviser to a senior politician. Mid-morning, I would feel shooting pains running up the back of my head, accompanied by waves of intense nausea. Soon afterwards, a deep ache in the base of my skull started, quickly spreading up over my head and into my temples. My eyes felt gritty, as if they were full of sand, and I yearned for them to explode to release the mounting pressure inside them.
Often when the pain was at its worst, I couldn’t think of the words I wanted to say, infuriating some colleagues. Sometimes I couldn’t string two words together coherently. My mouth refused to form the words I wanted to say, as if the messages weren’t getting through from my brain to the muscles in my face.
The Merry-Go-Round
Returning to Sydney in 1999, I despaired of ever being free of pain and nausea. I consulted an endless round of specialists and health professionals, but none of them helped much. I felt overwhelmed by head and neck pain and a general sense of ever-increasing pressure inside my head and eyes. I fantasized about boring a hole through the base of my skull with an electric drill to release the tension.
Between 2000 and 2005, I progressively stopped doing all the things I most loved because they triggered migraine attacks. My goal became getting through a day of work, returning home and lying in a dark room with a series of ice packs under my neck.
Anxiety about being stigmatized and the intolerance I perceived in some colleagues at work prevented me from admitting I was in pain. Instead, I worked like a Trojan to ensure I maintained a high level of performance and no one could accuse me of using pain as an excuse to under-perform.
While on the endless merry-go-round of seeking solutions, I ended up at the Michael J. Cousins Pain Management and Research Centre in Sydney. Dr. Cousins and a team of health professionals assessed me. They diagnosed occipital neuralgia, a form of headache that can activate migraine attacks. I had chronic pain, a malfunction in the way the nervous system processes pain signals.
The team suggested an experimental treatment. It involved implanting tiny electrodes into the back of my head and neck to block the pain signals from traveling along the nerves in my head. I agreed to the surgery and afterwards; I had fewer migraine attacks than previously. I even had a few completely pain-free days.
One year later, I felt something sharp sticking out from the base of my skull. My pain specialist discovered an electrode wire protruding through the skin. Tests revealed the electrodes were infected, so they were removed. Afterwards, migraine attacks returned in full force.
Three months later, new electrodes were implanted, but they didn’t work as well, possibly because scar tissue blocked transmission of the electric current. Still, overall I was better than before the initial surgery. I worked full time and sang in a choir at Sydney Opera House.
Disappointingly, disaster struck in 2008. A superbug infected the electrodes, forcing my doctor to remove them. Once the infection cleared and the electrodes were re-implanted, they were only partially successful, and my life returned to its pre-electrode state.
Multidisciplinary Pain Management
A significant turning point occurred in 2009 when I participated in a three-week multidisciplinary pain management program. Each day, a team of pain specialists gave lectures on topics such as chronic pain and how it differs from acute pain. The physiotherapists started us on a carefully graded exercise program, and a psychologist taught us cognitive behavioural therapy techniques to help us change the way we thought about and dealt with pain. Surprisingly, the exercises didn’t cause a flare-up and at last I felt as if I was making progress.
The pain management program taught me to stop catastrophizing and to believe I had the power to change how I reacted to pain. For years, I practiced the stretches and strengthening exercises every night after work. I also applied the psychological techniques, and they became central to my daily routine.
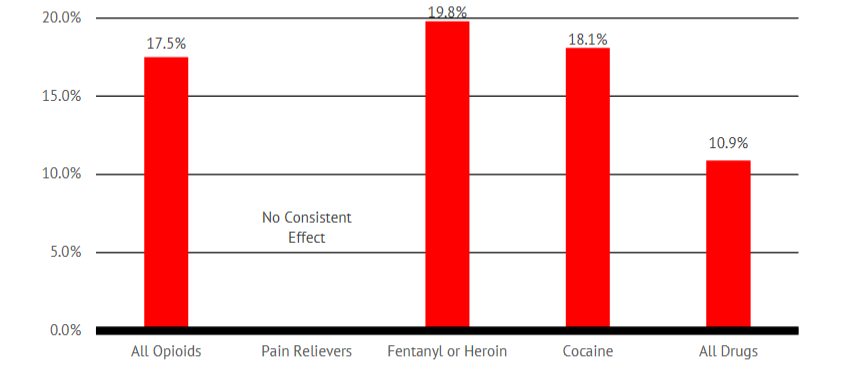
Twelve years later, I continue to live with migraine. I’ve tried several migraine preventatives, but none helped. Eight months ago, I started taking medicinal cannabis and it has significantly reduced the frequency and severity of migraine attacks.
Over the years I’ve learned to reduce the impact of migraine on my life by using techniques such as mindfulness meditation and carefully paced exercise that turn down the volume of pain signals racing through my malfunctioning nervous system.
Chronic pain is complex and difficult to treat but it is possible to live well with pain. I encourage you to do a multidisciplinary pain management program and continue your search for approaches that reduce the impact of pain on your life.
Gabriella Kelly-Davies is a biographer and studied biography writing at the University of Oxford, Australian National University and Sydney University. She recently authored “Breaking Through the Pain Barrier,” a biography of trailblazing Australian pain specialist Dr. Michael Cousins. Gabriella is President of Life Stories Australia Association and founder of Share your life story.